PCR074: The Primary Care COVID-19 Integrated Pathway: A Quantitative Study of Rapid Response to Health and Social Impacts of COVID-19
Fariba Aghajafari, MD, PhD, MSc; Kerry McBrien, MD, MPH; Jia Hu, MD, CCFP, MSc; Brian Hansen, MA, MPH; Alyssa Ness, MD, BN; Myles Leslie, PhD
Abstract
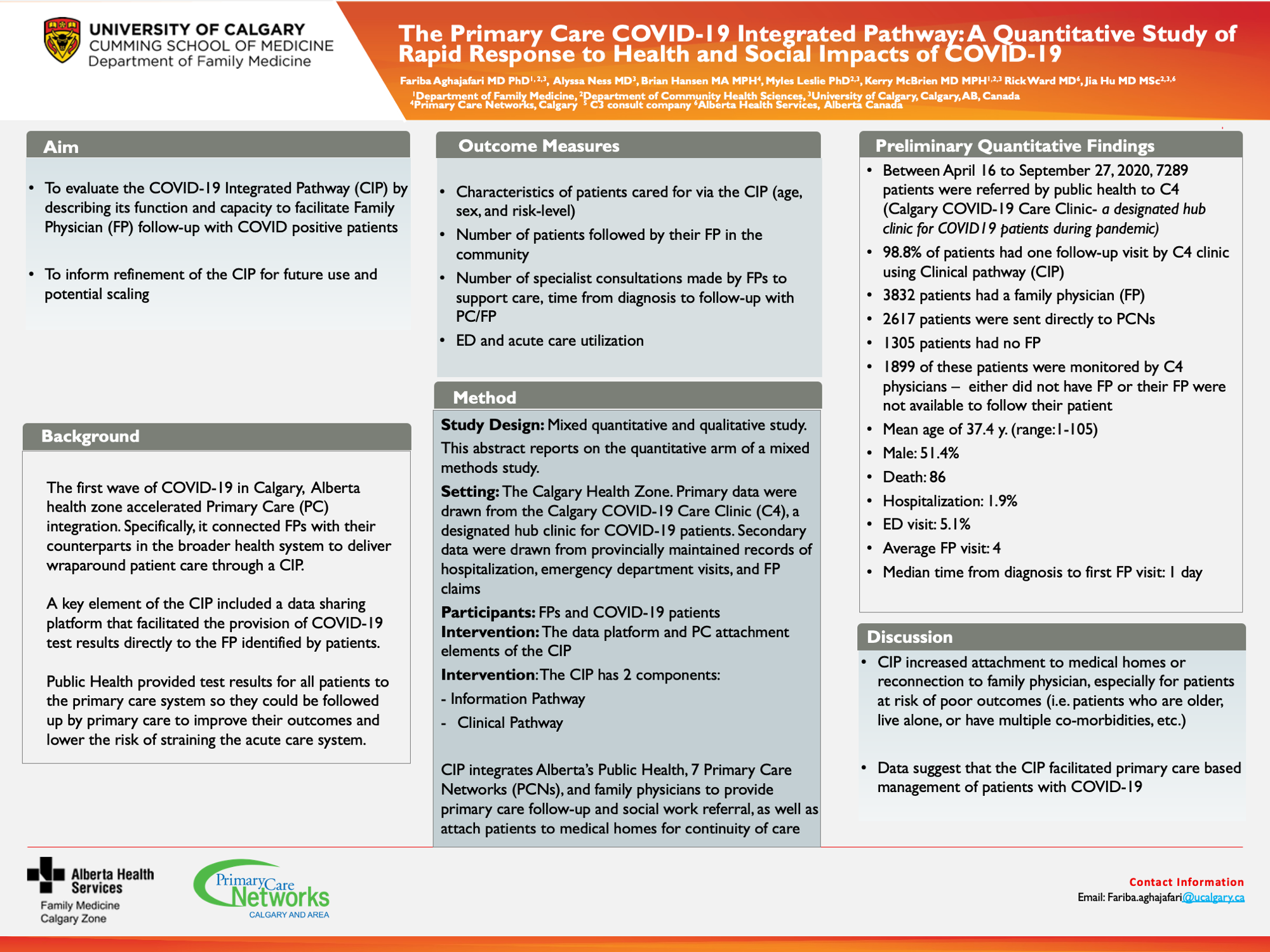
facilitated the provision of test results directly to the FP identified by patients. Public Health provided test results for all patients to the primary care system so they could be followed up by primary care to improve their outcomes. Objectives: To evaluate the CIP by describing its function and capacity to facilitate FP follow-up with COVID positive patients; and to inform refinement of the CIP for future use. Study Design: This abstract reports on the quantitative arm of a mixed methods study. Setting/ Dataset: The Calgary Health Zone. Primary data were drawn from the Calgary COVID-19 Care Clinic (C4), a designated hub clinic for COVID-19 patients. Secondary data were drawn from provincially maintained records of hospitalization, emergency department visits, and FP claims. Participants: FPs and COVID-19 patients. Intervention: The data platform and PC attachment elements of the CIP. Outcome Measures: The characteristics of patients cared for via the CIP (age, sex, ethnicity, and risk-level); the proportion of patients without a FP who were attached to an FP; the number of patients followed by their FP in the community, and the number of specialist consultations made by FPs to support care, time from diagnosis to follow-up with PC/FP; ED and acute care utilization. Results: Between Apr. 16 and Sep. 27, 2020, 7706 patients were referred by the Public Health team to the C4 clinic. Of those, 51.4% were male, the median age was 36 y., and 86 deaths were reported. The majority of patients were referred to local PC networks where follow-up was conducted using the CIP: 3223 (43%) already had their own FP, 2448 (32%) were successfully attached to an FP, and 1899 (25%) of these patients were monitored by C4 physicians – these patients either did not have FP or their FP was not available to follow the patient. 8.6% of these patients visited ED and 3.1% were hospitalized. More than 80% of these patients had at least of 5 visits with their FP. Conclusion: Data suggest that the CIP facilitated primary care based management of patients with COVID-19.
Jack Westfall
jwestfall@aafp.org 11/20/2021This is a great topic and research study. Nice work. Thanks