PCR021: COVID-19 Vaccination Hesitancy Among Southern Rural Veterans with Cancer in the Arkansas-Louisiana-Texas (ArkLATX) Region
Philip Haddad, MD, CHES, MHA, MPH; Dalia Hammoud, MD; Michelle Phelan, NP; Paige McGovern, BSN, RN, OCN, AMB-BC; Miriam McGowen, BSN, RN, OCN; Laura Houston, RN, OCN; Monica Craig, RN; Kevin Gallagher, MD
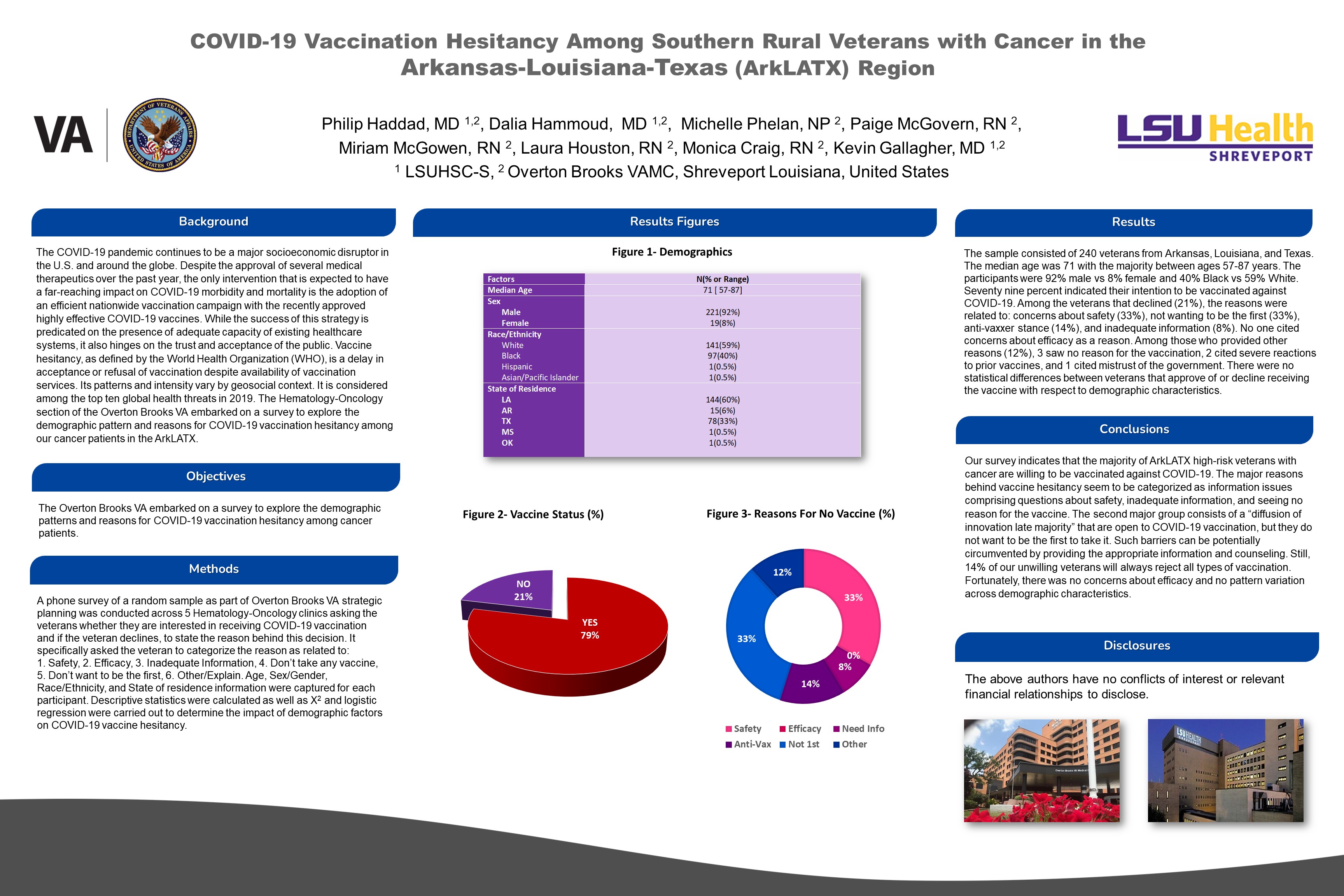
Context: The COVID-19 pandemic continues to be a major socioeconomic disruptor in the U.S. and around the globe. The only intervention that has a far-reaching impact is the adoption of an efficient large-scale vaccination campaign with the highly effective COVID-19 vaccines. While the success of this strategy is predicated on the presence of adequate healthcare systems capacity, it also hinges on the trust and acceptance of the public. Vaccine hesitancy, which varies by the geosocial context, is considered a top obstacle. Objective: The Overton Brooks VA embarked on a survey to explore the demographic patterns and reasons for COVID-19 vaccination hesitancy among cancer patients. Study Design: phone survey. Setting: five Hematology-Oncology clinics across the ArkLATX. Population: random sample of 240 veterans with cancer. Intervention: Veterans were asked whether they are interested in getting vaccinated and to state the reason if they declined. They were asked to categorize the reason as relating to safety, efficacy, inadequate Information, aversion to any vaccine, not wanting to be the first, or other/explain. Outcome Measures: 1. Descriptive statistics of those who want and those who decline the vaccine. 2. Determine the impact of demographic factors on COVID19 vaccine hesitancy. Results: The median age was 71 years. The participants were 92% males and 40% Black vs 59% White. Seventy nine percent wanted to get vaccinated. Among the veterans that declined (21%), the reasons were due to concerns about safety (33%), not wanting to be the first (33%), anti-vaxxer stance (14%), and inadequate information (8%). No one cited concerns about efficacy as a reason. Other reasons (12%) included seeing no reason for the vaccination, citing severe reactions to prior vaccines, and voicing mistrust of the government. There were no statistical differences between veterans that approved or declined the vaccine with respect to demographic characteristics. Conclusions: This survey indicates that the majority of ArkLATX veterans with cancer are willing to be vaccinated against COVID-19. The major reasons behind vaccine hesitancy seem to be information problems consisting of questions about safety, inadequate information, and seeing no reason for the vaccine. Such barriers can be potentially circumvented by providing the appropriate information and counseling.
Jack Westfall
jwestfall@aafp.org 11/19/2021Great poster and abstract. Thanks