PC05: Virtual Practice Facilitation Using the Analysis, Development, Design, Implement, Evaluate (ADDIE) Process Improvement Model
Shannon Peaden, MBA, CPF; Sanjeda Sultana MD, Angela Batchelor, RN, Denairina Smith, HIT
Abstract
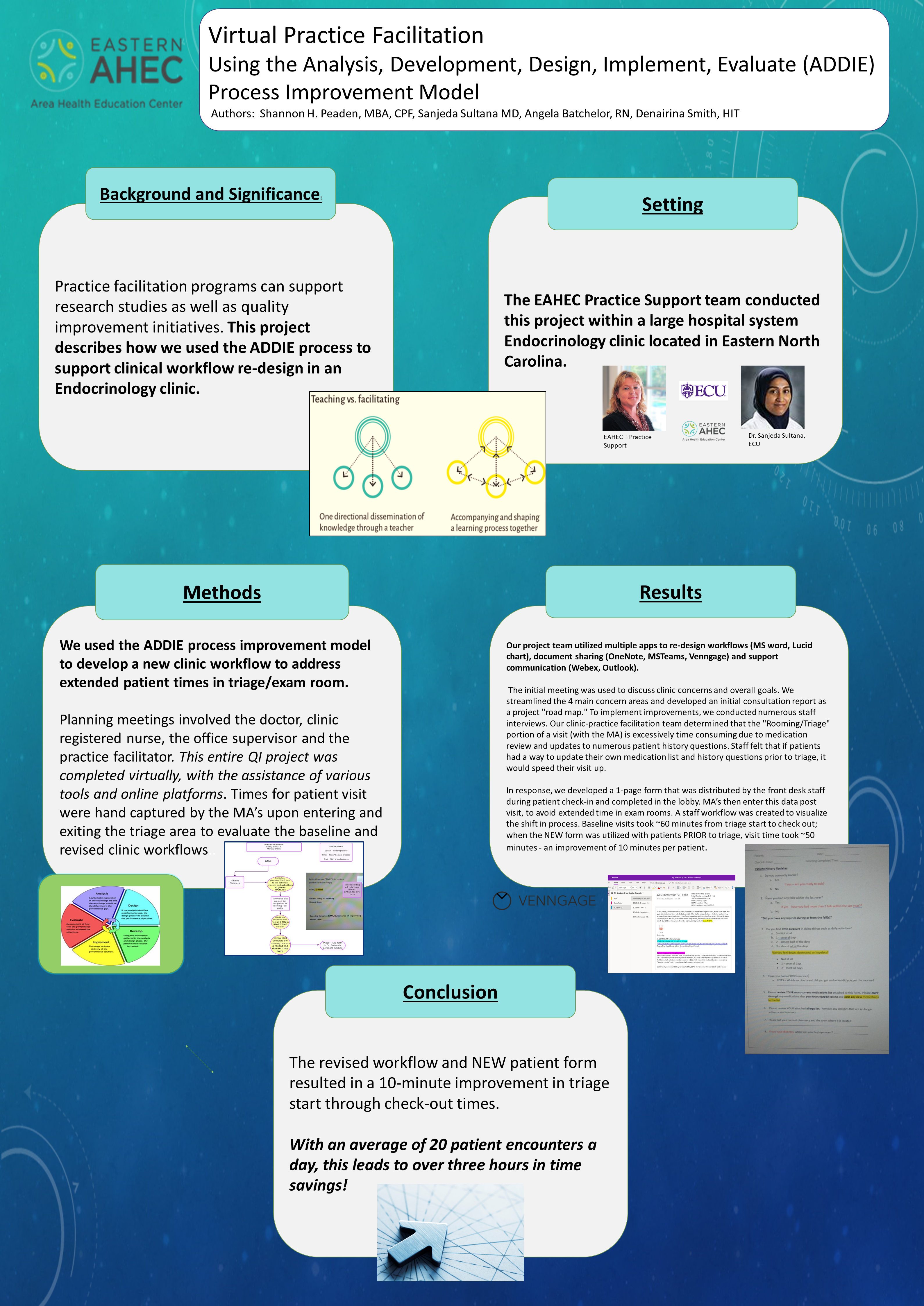
Background and Significance: Practice facilitation programs can support research studies as well as quality improvement initiatives. This project describes how we used the ADDIE process to support clinical workflow re-design in an Endocrinology clinic. Setting: The EAHEC Practice Support team conducted this project within a large hospital system Endocrinology clinic located in Eastern North Carolina. Methods: We used the ADDIE process improvement model to develop a new clinic workflow to address extended patient times in triage/exam room. Planning meetings involved the doctor, clinic registered nurse, the office supervisor and the practice facilitator. This entire QI project was completed virtually, with the assistance of various tools and online platforms. Times for patient visit were hand captured by the MA’s upon entering and exiting the triage area to evaluate the baseline and revised clinic workflows.. Results: Our project team utilized multiple apps to re-designed workflows (MS word, Lucid chart), document sharing (OneNote, MSTeams, Venngage) and support communication (Webex, Outlook). The initial meeting was used to discuss clinic concerns and overall goals. We streamlined the 4 main concern areas and developed an initial consultation report as a project "road map." To implement improvements, we conducted numerous staff interviews. Our clinic-practice facilitation team determined that the "Rooming/Triage" portion of a visit (with the MA) is excessively time consuming due to medication review and updates to numerous patient history questions. Staff felt that if patients had a way to update their own medication list and history questions prior to triage, it would speed their visit up. In response, we developed a 1-page form that was distributed by the front desk staff during patient check-in and completed in the lobby. MA’s then enter this data post visit, to avoid extended time in exam rooms. A staff workflow was created to visualize the shift in process. Baseline visits took ~60 minutes from triage start to check out; when the NEW form was utilized with patients PRIOR to triage, visit time took ~50 minutes - an improvement of 10 minutes per patient. Conclusion: The revised workflow and NEW patient form resulted in a 10-minute improvement in triage start through check-out times. With an average of 20 patient encounters a day, this leads to over three hours in time savings.
Gillian Bartlett (NACRG President)
gillian.bartlett@health.missouri.edu 8/5/2021Great work ! I really, really hope to see more work where PF get links to QI.