SRFP059: Impact of Virtual Morning Report on Learning and Well-being During the COVID-19 Pandemic
Thomas Quattlebaum, MD; Komal Soin, MD, MPH; Chien-Wen Tseng, MD, MPH, MS; Kayla Murata
Abstract
Objective: To evaluate whether a VMR improved training and decreased isolation.
Study Design: Cross-sectional anonymous online survey.
Setting: Community-based family medicine residency program
Population: All 21 residents, 5 clinical attendings, and 10 medical students interested in family medicine.
Intervention: A VMR held online 3 times weekly with interactive, clinical case-based presentations (30 minutes) by students, residents, and attendings including community physicians. Attendance was voluntary.
Main and Secondary Outcome Measures: Self-report of whether VMR improved medical knowledge and well-being.
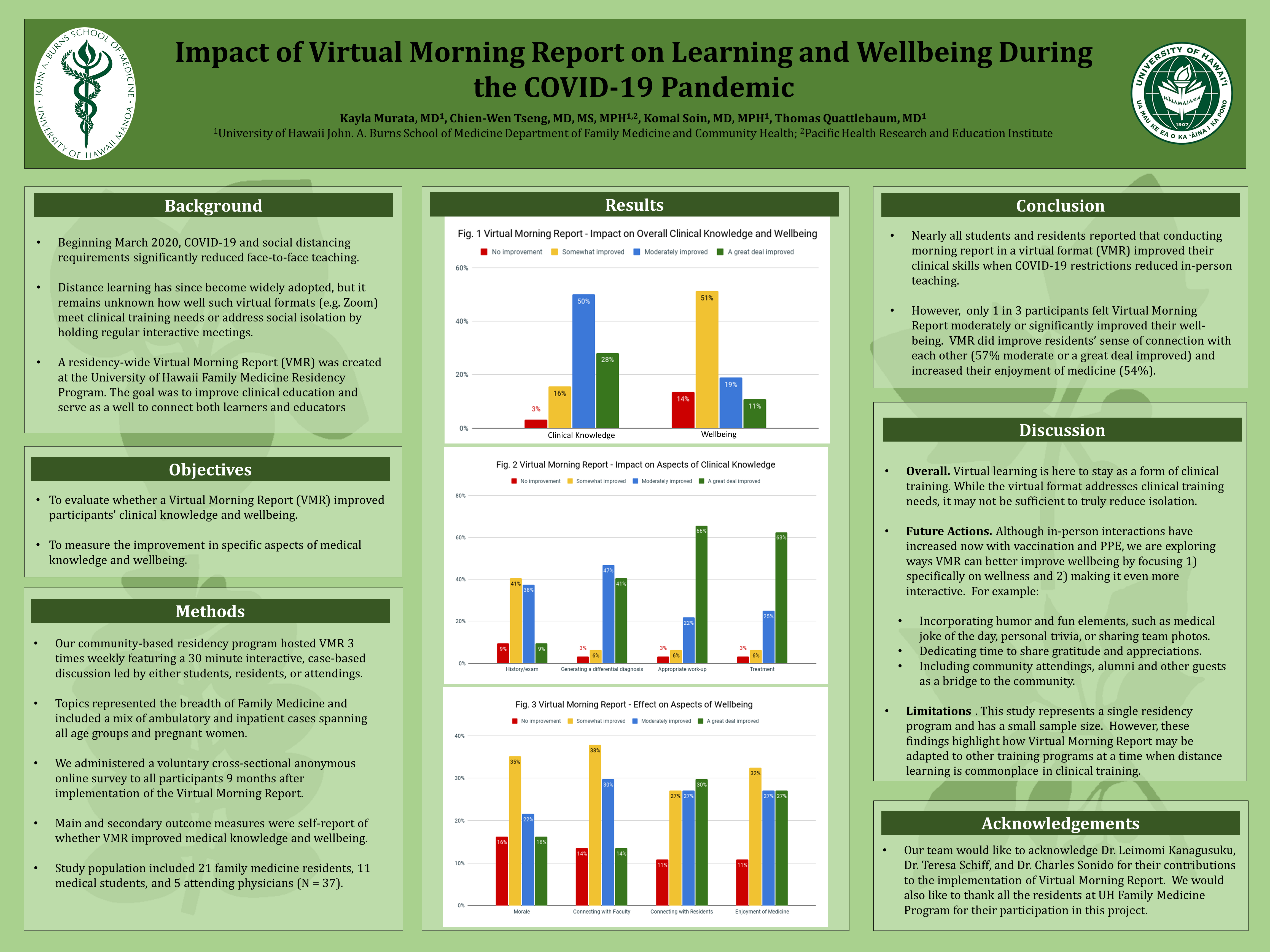
Results: Of the 37 participants (90% response), 87% reported that improving medical knowledge was a moderately or extremely important reason for attending VMR. Most reported that attending VMR improved their medical knowledge moderately or a great deal overall (78%), specifically for generating differential diagnoses (88%) and work-up (88%), and less so for history/exam (47%). With respect to social isolation, 62% reported improving well-being was an extremely or moderately important reason for attending VMR. Effect of VMR participation on social isolation was mixed with many but not all reporting that VMR improved their overall well-being moderately or a great deal (30%) by increasing morale (38%), enjoyment of medicine (54%), connecting with residents (57%), or connecting with faculty (44%).
Conclusions: Virtual Morning Reports proved to be an effective clinical training tool to improve medical knowledge when COVID-19 restrictions reduced in-person teaching. While participating in Virtual Morning Reports helped to improve well-being and increase a sense of connection through regular online socialization, more intentional efforts are needed to address the social isolation of students, residents, and attendings due to the COVID-19 pandemic.
Jack Westfall
jwestfall@aafp.org 11/21/2021Terrific project. Great poster and abstract. Thanks for sharing at NAPCRG