SRFP085: Racial disparity in the occurrence of suicides among patients with background Intimate Partner violence
Oluwasegun Akinyemi, MD, MS, FMCOG; Mary Fakorede, MD; Stella Adetokunbo; BOLARINWA AKINWUMI
Abstract
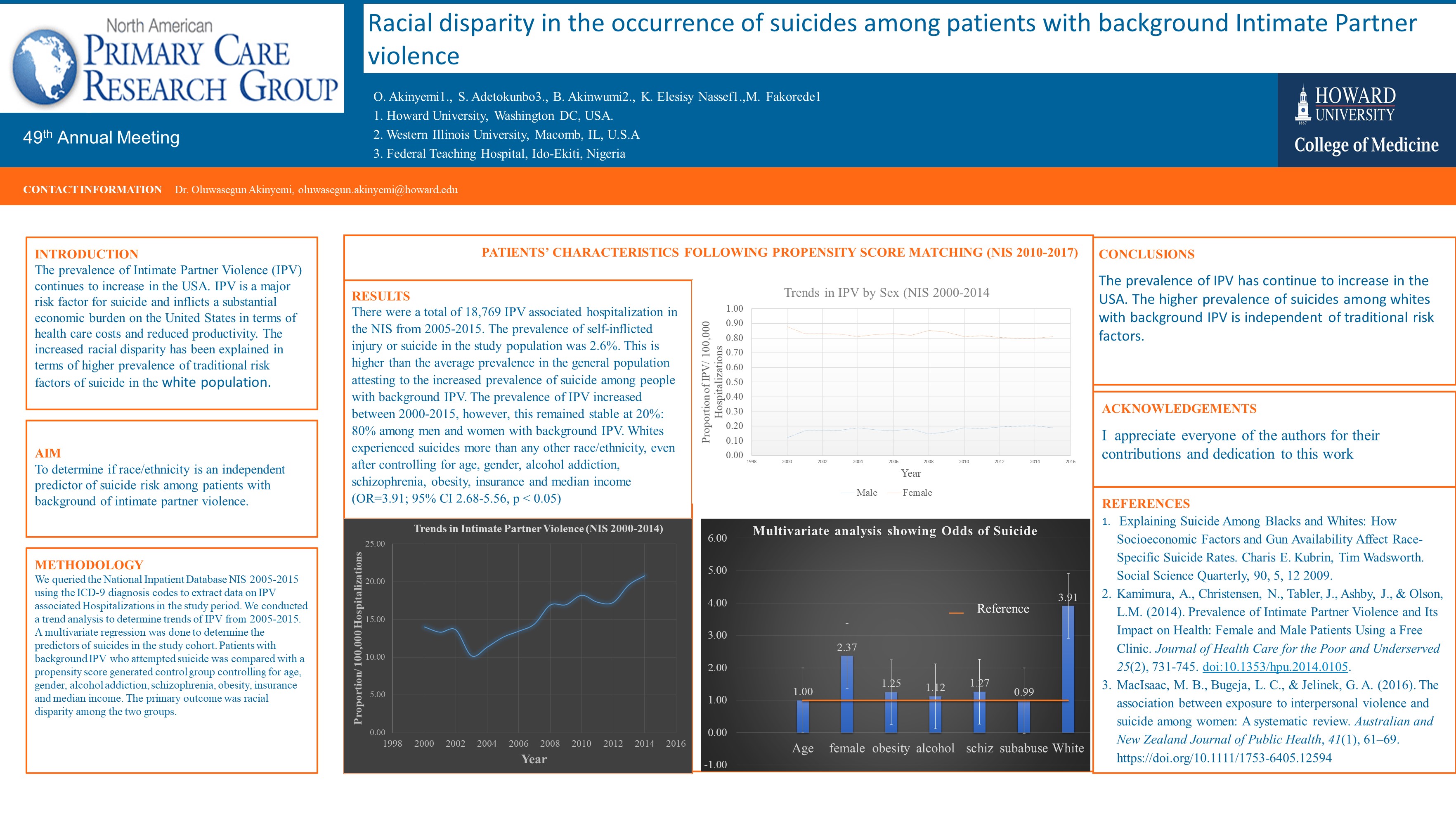
Aim: To determine if race/ethnicity is an independent predictor of suicide risk among women with background of intimate partner violence.
Method: We queried the National Inpatient Database NIS 2005-2015 using the ICD-9 diagnosis codes to extract data on IPV associated in the study period. We conducted a trend analysis to determine trends of IPV from 2005-2015. A multivariate regression was done to determine the predictors of suicides in the study cohort. Patients with background IPV who attempted suicide was compared with a propensity score generated control group controlling for age, gender, alcohol addiction, schizophrenia, obesity, insurance and median income. The primary outcome was racial disparity among the two groups.
Results: There were a total of 18,769 IPV associated hospitalization in the NIS from 2005-2015. The prevalence of self-inflicted injury or suicide in the study population was 2.6%. This is higher than the average prevalence in the general population attesting to the increased prevalence of suicide among people with background IPV. The prevalence of IPV increased between 2000-2015, however, this remained stable at 20%: 80% among men and women with background IPV. Whites experienced suicides more than any other race/ethnicity, even after controlling for age, gender, alcohol addiction, schizophrenia, obesity, insurance and median income (OR=3.87; 95% CI 2.68-5.56, p < 0.05).
Conclusion: The prevalence of IPV has continue to increase in the USA. The higher prevalence of suicides among whites with background IPV is independent of traditional risk factors.
Jack Westfall
jwestfall@aafp.org 11/21/2021Thanks for your terrific work on this research. Hope we can connect at the Robert Graham Center in DC. thanks