SRFP072: Outpatient Antibiogram and Predictors of Ciprofloxacin and Trimethoprim-Sulfamethoxazole Resistant Urinary Tract Infections
Marissa Valentine-King, PhD, BSN, MPH, RN; Roger Zoorob, MD, MPH; Barbara Trautner, MD, PhD; Larissa Grigoryan, MD, PhD
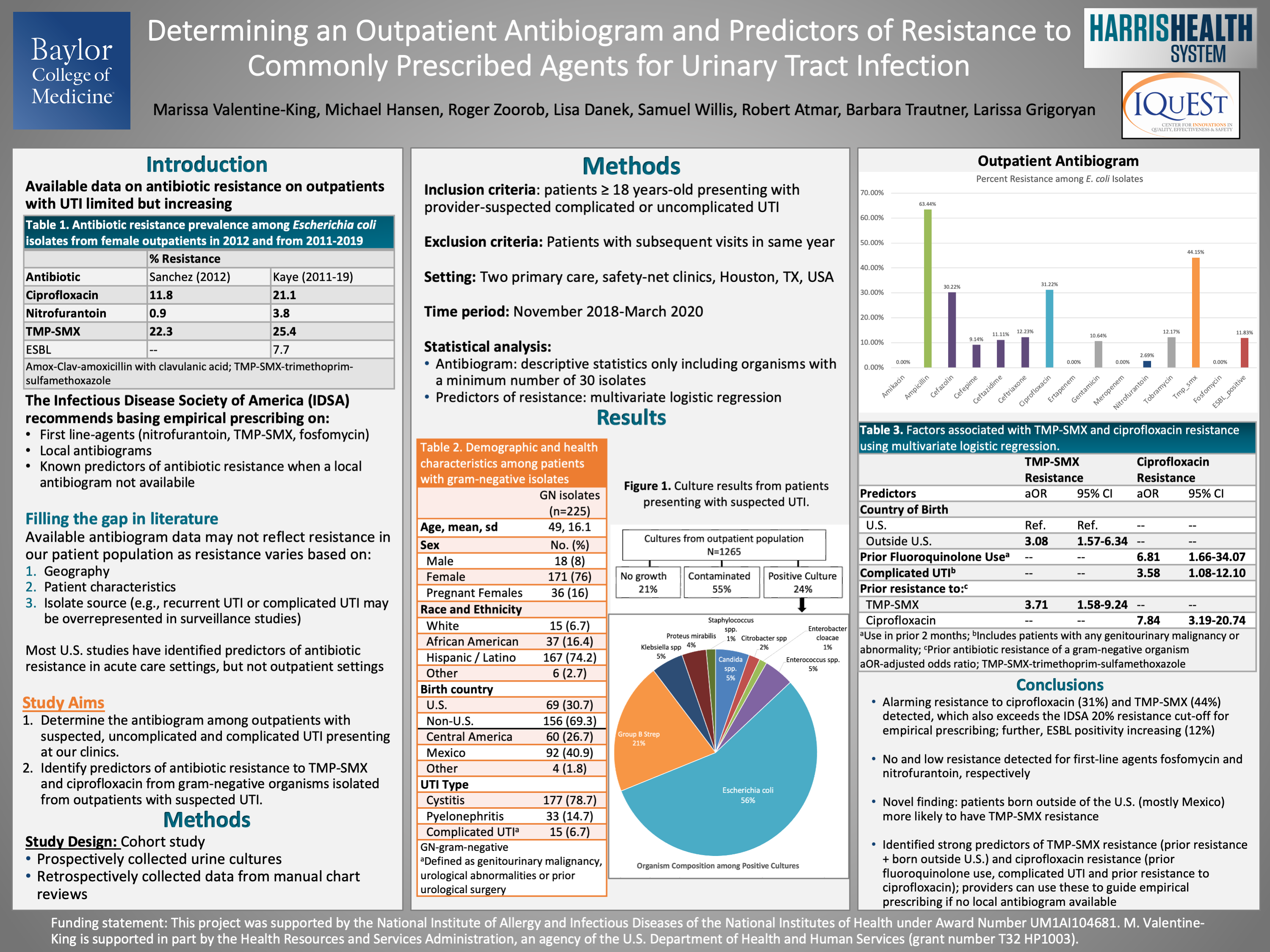
Context: Rising antibiotic resistance has transcended hospital boundaries and impacted individuals with community acquired urinary tract infections (UTI). Scant data on antibiotic resistance in outpatient settings exists and most studies in the United States (U.S.) have identified predictors of resistance in acute-care settings. Objective: Determine the antibiogram among Escherichia coli isolates and factors associated with ciprofloxacin and trimethoprim-sulfamethoxazole (TMP-SMX) resistant gram-negative urinary isolates. Study Design: Retrospective cohort study. Setting: Two primary care, safety-net clinics in Houston, TX between 11/2018 and 3/2020. Population studied: Patients aged 18 and older presenting with provider suspected uncomplicated or complicated UTI. Outcome measures: Resistance and predictors of resistance to UTI-relevant antibiotics. Results: Among 1265 cultures collected, 372 (28.4%) were positive. We detected E. coli (50.3%) and Group B Streptococcus (18.6%) most frequently. Our patient population consisted mostly of Hispanic (75.7%) females (92.5%) born outside the U.S. (67.3%) with a mean age of 47. Among patients with E. coli isolated (n=189), antibiotic resistance was highest to ampicillin (63%), TMP-SMX (44%), ciprofloxacin (31%), and cefazolin (30%); no or low resistance against amikacin (0%), fosfomycin (0%), and nitrofurantoin (2.7%) was detected. Approximately 12% of E. coli isolates were extended-spectrum beta-lactamase positive. Having a prior UTI caused by a TMP-SMX resistant gram-negative organism and being born outside the U.S increased the odds of TMP-SMX resistance by 3.71 (95% confidence interval:1.6-9.2) and 3.08 (95% CI: 1.6-6.3), respectively. Having a complicated UTI (odds ratio (OR): 3.58; 95% CI: 1.1-12.1), prior fluoroquinolone use (OR: 6.81; 95% CI: 1.7-34.1) and a prior UTI with ciprofloxacin resistance (OR: 7.84; 95% CI: 3.2-20.7) increased the odds of having a ciprofloxacin resistance. Conclusion: The Infectious Disease Society of America cautions against prescribing an antibiotic if regional resistance exceeds 20%. We constructed an antibiogram and found resistance surpassed this threshold for TMP-SMX and ciprofloxacin and identified factors associated with resistance to these agents. Assessing these characteristics during clinical decision making may improve antibiotic-organism susceptibility concordance in primary care.
Jack Westfall
jwestfall@aafp.org 11/21/2021Terrific poster and presentation. Thanks for your work. and thanks for sharing at NAPCRG. i keep learning new things, every year.