SRFP082: Providers Perceptions of Barriers and Facilitators to Caring for Patients and Self during the COVID-19 Pandemic
Katherine O'Hare, MSW; Whitney Schwalm, BA; Hazel Tapp, PhD, PhD; Imani Abrahamsen, BS; Crystal Johnson, BA; Samip Patel, BS; Jonisha Brown, MD, Brown; Rebecca Beesley, MD, MPH; Michael Steinbacher
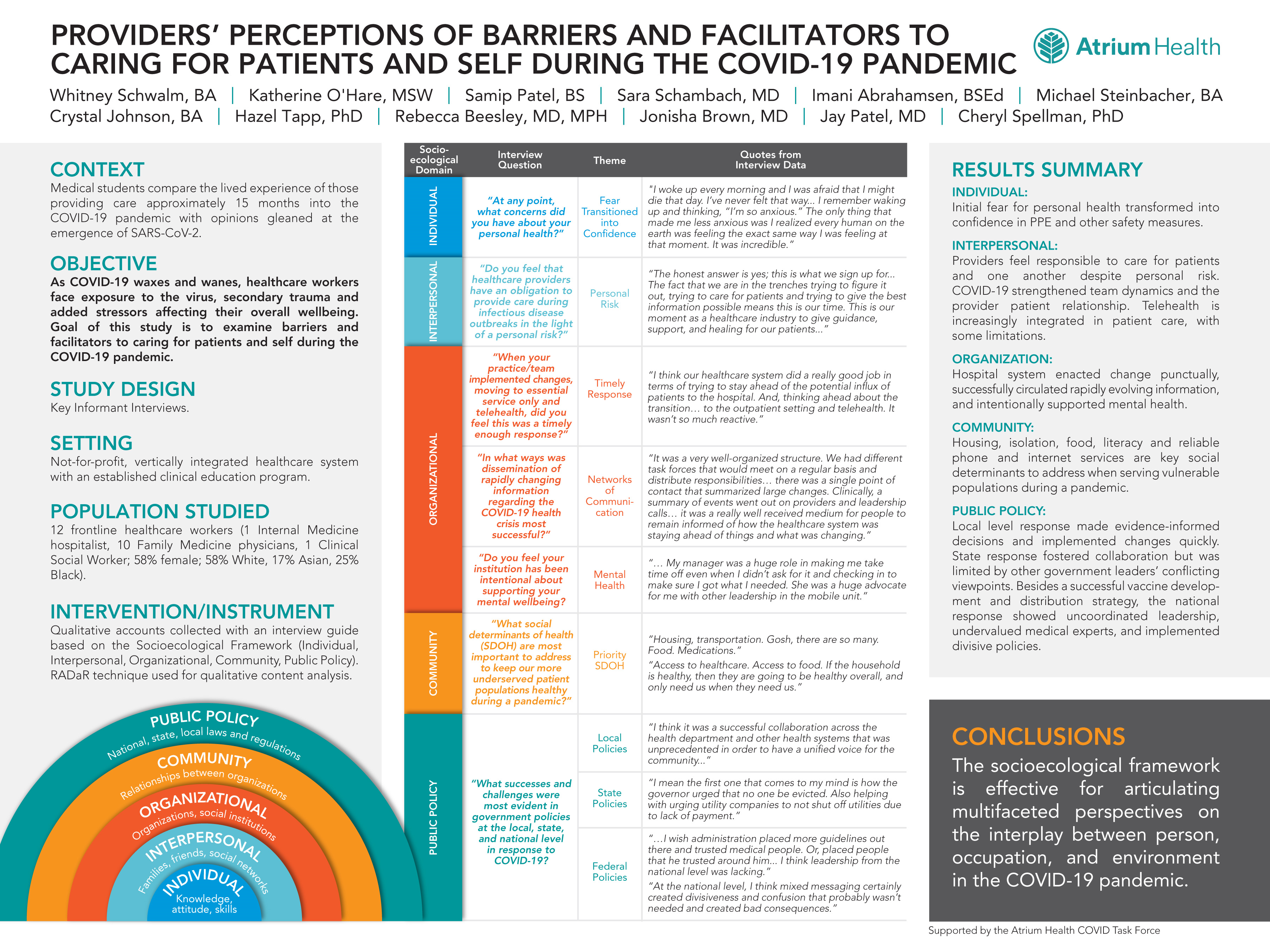
Context: In a second round of data collection, medical students compare the lived experience of those providing care approximately 15 months into the COVID-19 pandemic with opinions gleaned at the emergence of SARS-CoV-2. As COVID-19 waxes and wanes, healthcare workers face exposure to the virus, secondary trauma and added stressors, affecting their overall wellbeing and ability to remain present when caring for patients. Objective: To illuminate barriers and facilitators to caring for patients and self during the COVID-19 pandemic. Study Design: Key Informant Interviews. Setting: Not-for-profit, vertically integrated healthcare system with an established clinical education program. Population studied: 12 frontline healthcare workers (1 Internal Medicine hospitalist, 10 Family Medicine physicians, 1 Clinical Social Worker; 58% female, 58% White, 17% Asian, 25% Black). Intervention/Instrument: Qualitative accounts collected with an interview guide based on the Socioecological Framework domains (Individual, Interpersonal, Organization, Community, Public policy) and analyzed using the RADaR technique. Outcome Measures: Evaluate provider perceptions of practicing during COVID-19. Results: Individual: Initial fear for personal health transformed into confidence in PPE and other safety measures. Interpersonal: Providers feel responsible to care for patients and one another despite personal risk. COVID-19 strengthened team dynamics and the provider patient relationship. Telehealth is increasingly integrated in patient care, with some limitations. Organization: hospital system enacted change punctually, successfully circulated rapidly evolving information, and intentionally supported mental health. Community: Access to PPE, housing, isolation, food, literacy and reliable phone and internet services are key social determinants to address when serving vulnerable populations during a pandemic. Public policy: local level response made evidence-informed decisions and implemented changes quickly. State response fostered collaboration but was limited by other government leaders’ conflicting viewpoints. Besides a successful vaccine development and distribution strategy, the national response showed uncoordinated leadership, undervalued medical experts, and implemented divisive policies. Conclusions: The socioecological framework is effective for articulating multifaceted perspectives on the interplay between person, occupation, and environment in the COVID-19 pandemic.
Jack Westfall
jwestfall@aafp.org 11/21/2021Terrific project. Great poster and abstract. Thanks for sharing at NAPCRG