SRFP038: Evaluating Rural-Urban Differences in Burnout Among Primary Care Professionals During COVID-19
Jessica Clifton, PhD; Levi Bonnell, MPH, PhD Candidate; Niranjana Das; Juvena Hitt, MPH; Gail Rose, PhD; Benjamin Littenberg, MD; Constance van Eeghen, DrPH, MHSA; Lisa Natkin, PhD; Sarah Cooper, BS
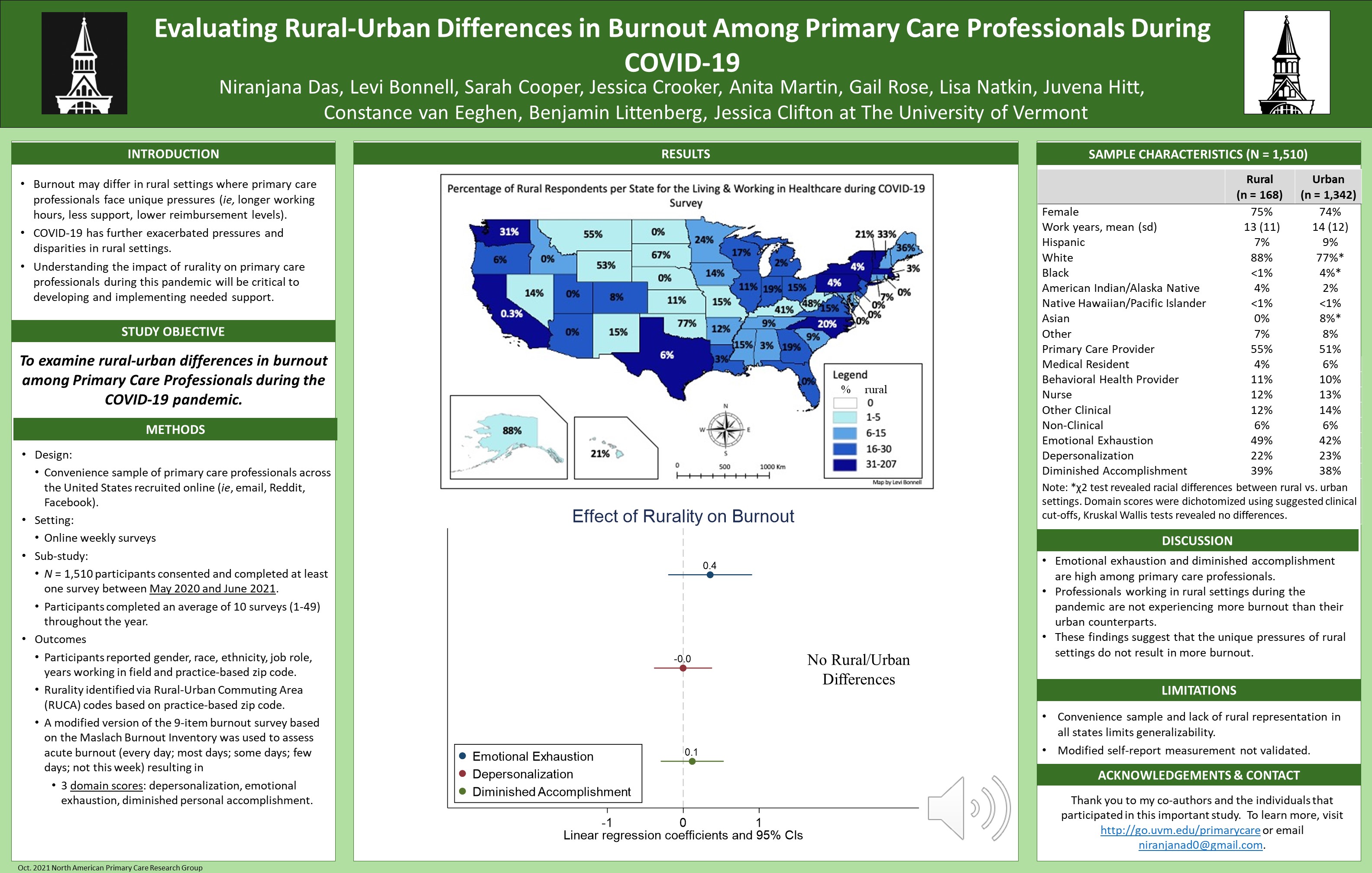
Context: Primary care professionals in rural settings face unique pressures (ie, lower reimbursement, longer working hours, less support, more patient visits, and a greater proportion of patients with poorer health) that may result in more burnout. COVID-19 has further exacerbated these pressures and disparities. Understanding the impact of rurality on primary care professionals during this pandemic will be critical to developing and implementing mitigating supports. Objective: To examine rural-urban differences in burnout among primary care professionals during COVID-19. Study Design: Online weekly surveys. Setting: Convenience sample of professionals across the US recruited through online platforms (ie, email, Reddit, Facebook). Population Studied: 1,509 professionals working in the US consented and completed at least one survey between May 2020 and June 2021. Main and Secondary Outcome Measures: Participants reported gender, race, job role (ie, medical provider, nurse, behavioral health, medical assistant, administrative support), years working in the field and practice-based zip code. A modified version of a nine-item measurement based on the Maslach Burnout Inventory was included resulting in three domains: depersonalization, emotional exhaustion, and diminished personal accomplishment. Scores ranged between 0-12. A total domain score was calculated by dichotomizing the domain scores using suggested clinical cut-offs. Rurality was identified via Rural-Urban Commuting Area (RUCA) codes based on zip code. Anticipated Results: Participants total burnout rates upon first survey were 66% (n = 166) in rural vs. 61% (n = 1,343) in urban settings. Mixed linear regression analyses clustered on participants adjusting for confounders (gender, race, role, years working in the field) revealed a significant rural-urban difference in exhaustion (B = 0.48, 95% CI 0.01 to 0.96, P = 0.047), but not depersonalization (B = 0.01, 95% CI -0.31 to 0.32, P = 0.974) or accomplishment (B = 0.07, 95% CI –0.29 to 0.44, P = 0.692). Conclusions: Echoing previous findings, burnout among primary care professionals is high. Professionals working in rural settings during this pandemic may be experiencing slightly more exhaustion than their urban counterparts. Understanding this relationship would enable leaders and policymakers to provide targeted supports for the professionals that are the backbone of healthcare to rural Americans.
Jack Westfall
jwestfall@aafp.org 11/21/2021Terrific poster and presentation. Thanks for your work.