SRFP073: Outpatient COVID19 diagnosis and subsequent thromboembolic events
Kate Schreck, MD, BA; Jason Ricco, MD, MPH
Abstract
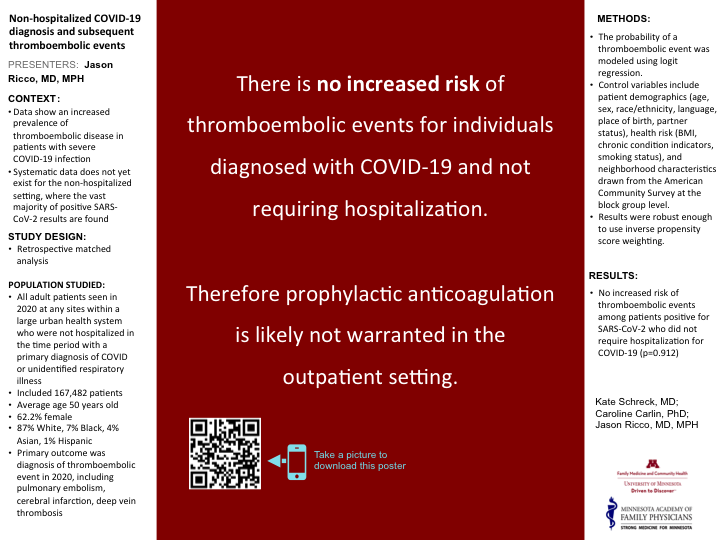
Objective: What is the incidence proportion of thromboembolic events, including DVT, PE, CVA, among non-hospitalized patients diagnosed with COVID?
Study Design: Retrospective matched analysis
Population Studied: All adult patients seen in 2020 at any sites within a large urban health system who were not hospitalized in the time period with a primary diagnosis of COVID or unidentified respiratory illness. This included 168,089 patients. Average age was 50 years old and 62.2% were female. 87% White, 7% Black, 4% Asian, 1% Hispanic.
Main Outcome Measure: Diagnosis of thromboembolic event in 2020, including pulmonary embolism, cerebral infarction, deep vein thrombosis
Results: Preliminary results suggest there is no increased risk of thromboembolic events among patients positive for SARS-CoV-2 who did not require hospitalization for COVID.
Conclusions: Preliminary results suggest there is no increased risk of thromboembolic events for outpatient COVID19 diagnosis and therefore prophylactic anticoagulation is likely not warranted in the outpatient setting.
Learning Objective: On completion of this session, participants should be able to (1) describe the risk of thromboembolic events after COVID19 diagnosis and (2) explain the appropriate use of prophylactic anticoagulation therapy in the setting of COVID19 diagnosis.
Jack Westfall
jwestfall@aafp.org 11/21/2021Every year at NAPCRG i learn something new. thanks for your work, research, poster, and for sharing at NAPCRG.