SRFP001: 6-month evaluation of a pilot patient navigator program for people experiencing homelessness lasting 3-to-7 weeks in duration
Camille Powers; Nora Gimpel, MD; Glaiza-Mae Sande-Docor; Kristine Yang, BS; Robyn Scott; Jonathan Tao; Aziz Shaaban, BS; Shelley Speed, FNP, MSN, ACNP-BC, FNP-BC; Heather Lanier, MPH
Abstract
Objective: SCS has been working with clients on a small scale for 6 months, and this study aims to evaluate program design and readiness to implement on a larger scale.
Study Design: Case review of 12 men who participated in the SCS program after recommendation by shelter chaplains.
Setting: Men experiencing homelessness living in a large shelter in Dallas, Texas.
Population studied: Adult men experiencing homelessness and living at local shelter in Dallas, Texas.
Intervention: The six navigator teams, each consisting of two trained students, meets with their client once per week and develops one to two SMART (specific, measurable, actionable, realistic, and time-bound) goals based on the client’s acute social or health-related needs.
Main Outcome Measures: The primary outcomes include the number of successful patient-navigator encounters and completion of goals.
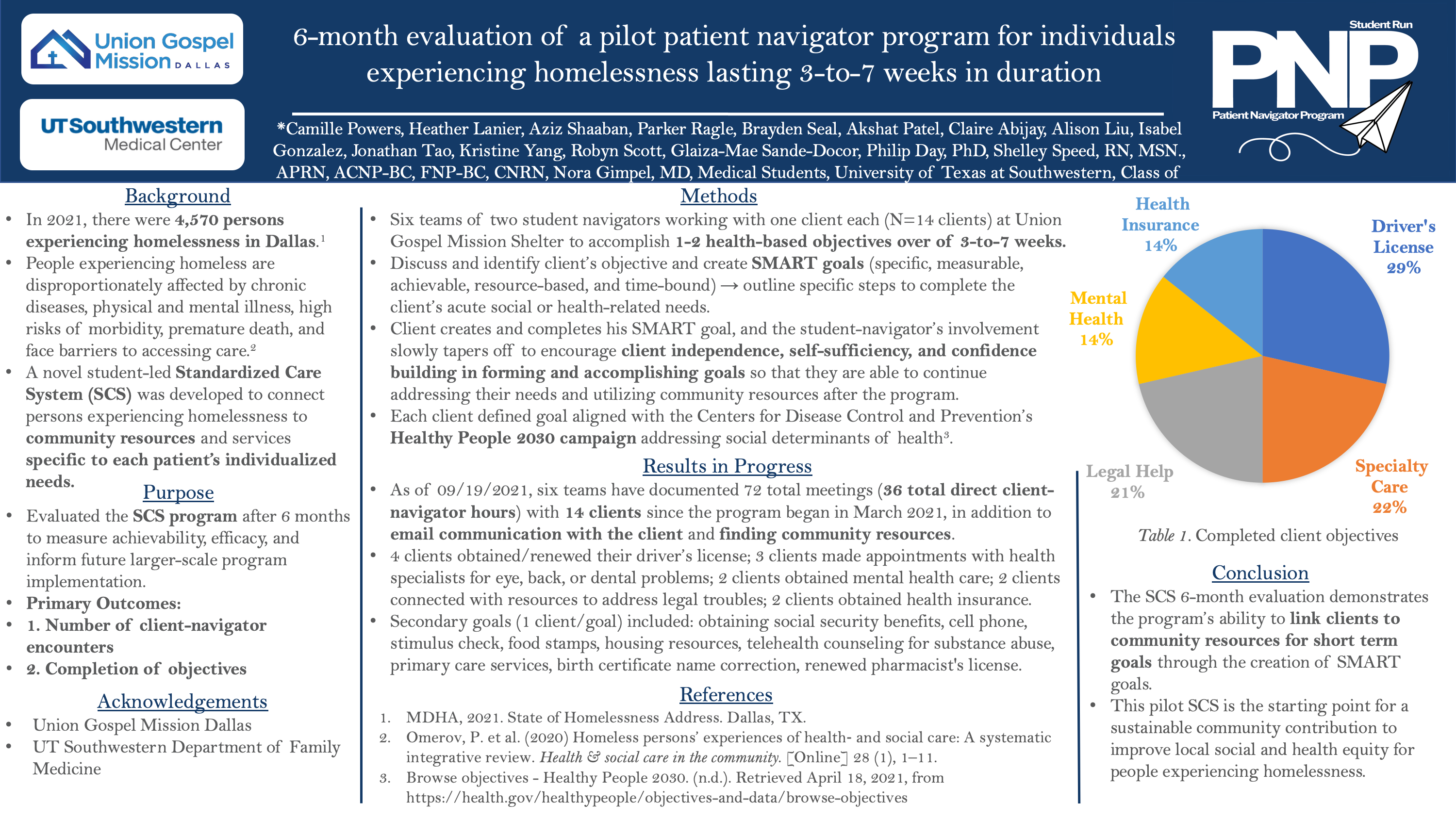
Results: SCS teams met weekly for 3 to 7 weeks, amounting to 59 meetings averaging 30 minutes each for 29.5 hours total of direct client interaction. Four clients obtained or renewed their driver’s license; three clients made appointments with health specialists for eye, back, or dental problems; two clients obtained mental health care; two clients connected with resources to address legal troubles; and one client each obtained health insurance, social security benefits, cell phone, stimulus checks, food stamps, housing, telehealth counseling services for substance abuse evaluation, primary care services, birth certificate name correction, and renewed a pharmacist license. These addressed multiple of the Centers for Disease Control and Prevention’s (CDC) Healthy People 2030 (HP2030) objectives including: AHS-R02, AHS-04, AHS-05, AHS-06, AHS-07, SDOH-01, MHMD-R01.
Conclusions: We saw successful completion of patient’s individualized SMART goals to improve health outcomes. This 6-month trial of SCS is a starting point for a sustainable community contribution to improve local social and health equity for people experiencing homelessness.
Jack Westfall
jwestfall@aafp.org 11/21/2021Terrific project. Great poster and abstract. Thanks for sharing at NAPCRG