SRFP086: Racial Health Equity in VA Transitions Between Maternity and Primary Care
Megha Shankar, MD; Divya Gopisetty; Jonathan Shaw, MD, MS; Caroline Gray, PhD; Ciaran Phibbs, PhD
Abstract
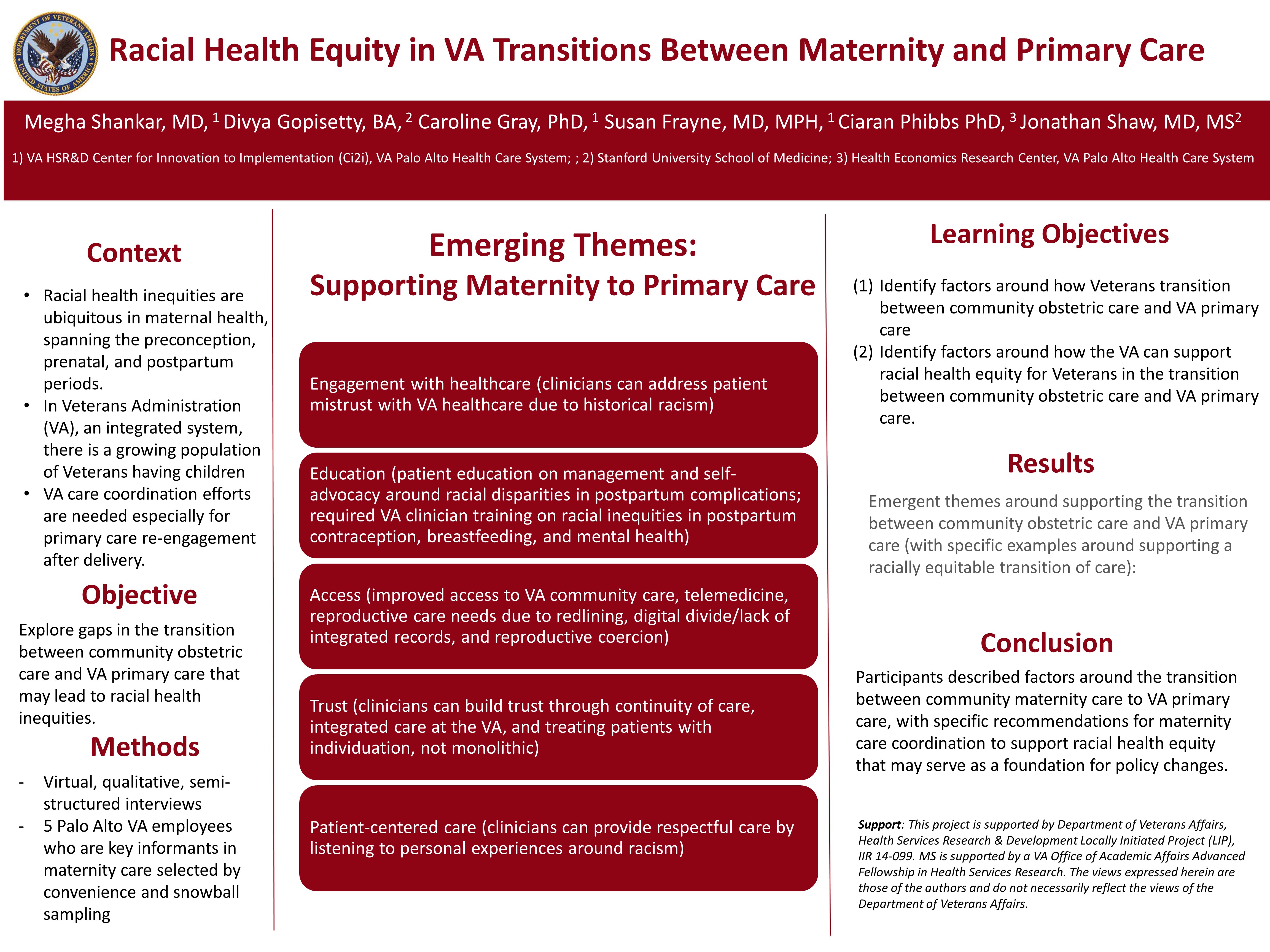
Context: Racial health inequities are ubiquitous in maternal health and span the preconception, prenatal, and postpartum periods. In Veterans Administration (VA), there is a growing population of Veterans having children. As an integrated system, yet one without obstetric care, the VA is poised to serve Veterans through the arc of their pregnancy, via explicit care coordination efforts and particularly VA primary care re-engagement after delivery. Prior quantitative work demonstrated racial/ethnic gaps in primary care re-engagement at the VA, and there is a need to explore the reasons for these gaps in care.
Objective: Explore gaps in the transition between community obstetric care and VA primary care that may lead to racial health inequities.
Study Design: Qualitative study
Setting or Dataset: Virtual, semi-structured interviews
Population Studied: 5 Palo Alto VA employees who are key informants in maternity care/women’s health selected by convenience and snowball sampling.
Main and Secondary Outcome Measures (if any): Themes around racial health equity in the transition between community obstetric care and VA primary care.
Results: Participants discussed emerging themes around supporting the transition between community obstetric care and VA primary care (with specific examples around supporting a racially equitable transition of care):
1. Engagement with healthcare (clinicians can address patient mistrust with VA healthcare due to historical racism)
2. Education (patient education on management and self-advocacy around racial disparities in postpartum complications; required VA clinician training on racial inequities in postpartum contraception, breastfeeding, and mental health)
3. Access (improved access to VA community care, telemedicine, reproductive care needs due to redlining, digital divide/lack of integrated records, and reproductive coercion)
4. Trust (clinicians can build trust through continuity of care, integrated care at the VA, and treating patients with individuation, not monolithic)
5. Patient-centered care (clinicians can provide respectful care by listening to personal experiences around racism)
Conclusions: Participants described factors around the transition between community maternity care to VA primary care, with specific recommendations for maternity care coordination to support racial health equity that may serve as a foundation for policy changes.
Objective: Explore gaps in the transition between community obstetric care and VA primary care that may lead to racial health inequities.
Study Design: Qualitative study
Setting or Dataset: Virtual, semi-structured interviews
Population Studied: 5 Palo Alto VA employees who are key informants in maternity care/women’s health selected by convenience and snowball sampling.
Main and Secondary Outcome Measures (if any): Themes around racial health equity in the transition between community obstetric care and VA primary care.
Results: Participants discussed emerging themes around supporting the transition between community obstetric care and VA primary care (with specific examples around supporting a racially equitable transition of care):
1. Engagement with healthcare (clinicians can address patient mistrust with VA healthcare due to historical racism)
2. Education (patient education on management and self-advocacy around racial disparities in postpartum complications; required VA clinician training on racial inequities in postpartum contraception, breastfeeding, and mental health)
3. Access (improved access to VA community care, telemedicine, reproductive care needs due to redlining, digital divide/lack of integrated records, and reproductive coercion)
4. Trust (clinicians can build trust through continuity of care, integrated care at the VA, and treating patients with individuation, not monolithic)
5. Patient-centered care (clinicians can provide respectful care by listening to personal experiences around racism)
Conclusions: Participants described factors around the transition between community maternity care to VA primary care, with specific recommendations for maternity care coordination to support racial health equity that may serve as a foundation for policy changes.
Jack Westfall
jwestfall@aafp.org 11/21/2021Great poster and abstract. Thanks for sharing at NAPCRG