SRFP108: Trauma Informed Approaches in VA Peripartum Care
Divya Gopisetty; Jonathan Shaw, MD, MS; Megha Shankar, MD; Caroline Gray, PhD; Ciaran Phibbs, PhD
Abstract
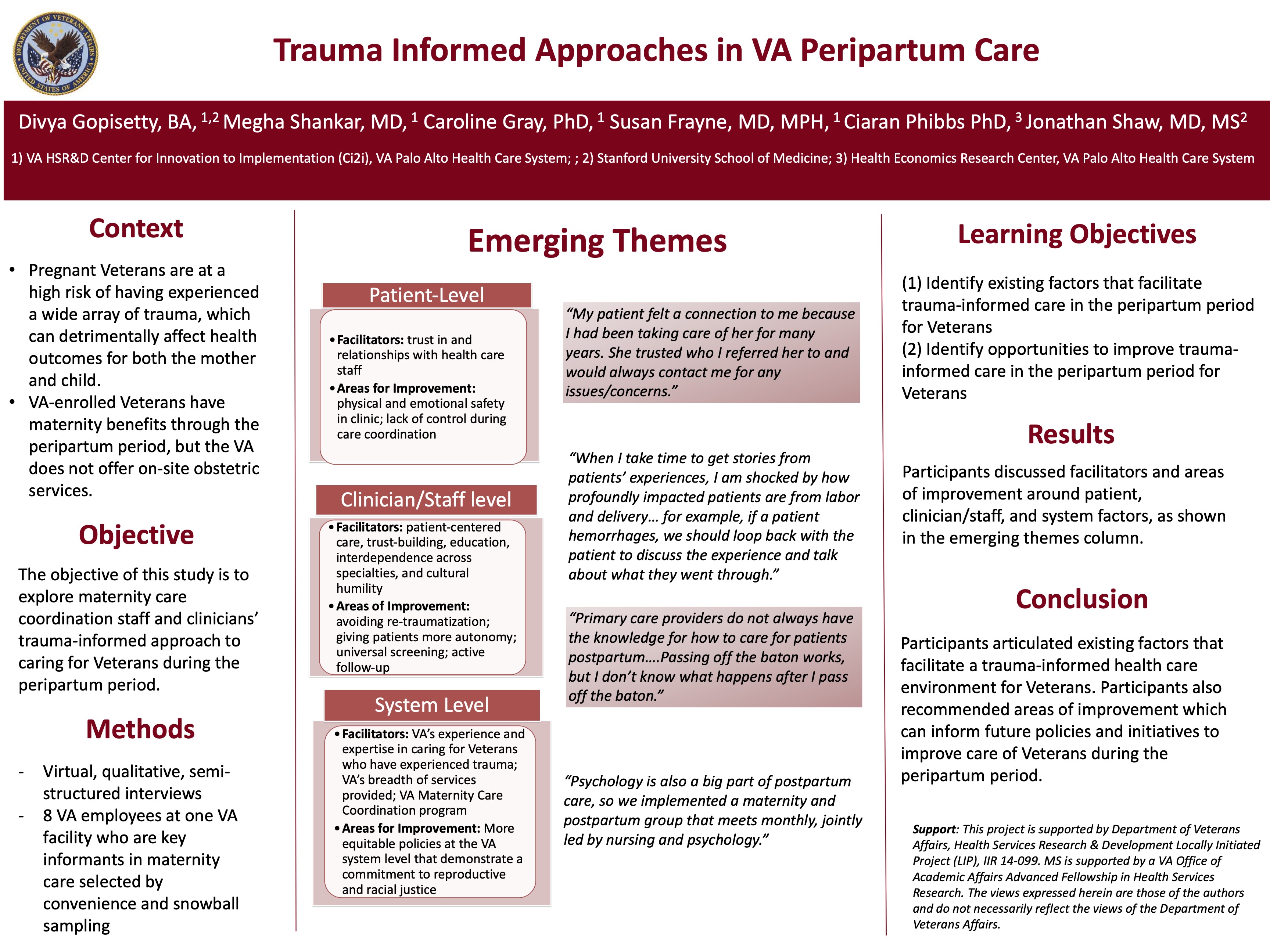
Objective: The objective of this study is to explore maternity care coordination staff and clinicians’ trauma-informed approach to caring for Veterans during the peripartum period.
Study Design: Semi-structured qualitative interviews
Dataset: We conducted five in-depth interviews with key maternity care staff informants affiliated with the Palo Alto VA. All participants were selected through an intentional sampling approach.
Main and Secondary Outcome Measures: Identification of facilitators and potential areas of improvement related to trauma-informed care in the peripartum period
Anticipated Results: Participants discussed facilitators and areas of improvement around patient, clinician/staff, and system factors:
1. At the patient-level:
- Facilitators: trust in health care staff
- Areas of improvement: physical and emotional safety in clinic; lack of control during care coordination
2. At the clinician/staff level:
- Facilitators: patient-centered care, trust-building, education, interdependence across specialities, and cultural humility
-Areas for improvement: avoiding re-traumatization; giving patients more autonomy; universal screening; active follow-up
3. At the system-level:
- Facilitators: VA’s experience and expertise in caring for Veterans who have experienced trauma; VA’s breadth of services provided; VA Maternity Care Coordination program
- Areas for improvement: More equitable policies at the VA system level that demonstrate a commitment to reproductive and racial justice
Conclusions: Participants articulated existing factors that facilitate a trauma-informed health care environment for Veterans. Participants also recommended areas of improvement which can inform future policies and initiatives to improve care of Veterans during the peripartum period.
Jack Westfall
jwestfall@aafp.org 11/21/2021Terrific poster and presentation. Thanks for your work.