SRFP042: Exploring COVID-19 vaccination decision-making process at a FQHC serving primarily Spanish-speaking patients
Charlotte Crider, BA; Ana Salgado; Cindy Aguilar-Hernandez; Kathleen DiPasquale Seelig
Abstract
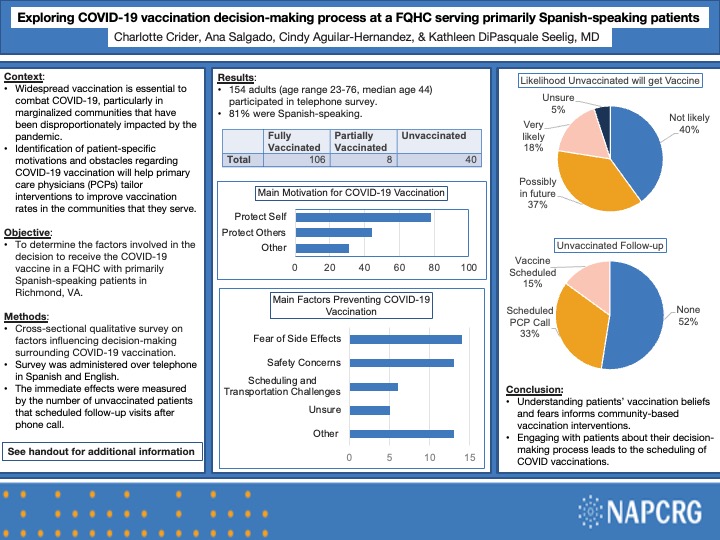
Context: The COVID-19 pandemic has disproportionately impacted marginalized communities in the United States, including the Latinx community. Widespread vaccination is essential to prevent further morbidity and mortality, yet each patient has their own understanding of the benefits and risks of COVID-19 vaccination. This quality improvement project explores the decision to receive or not to receive the COVID-19 vaccine in patients at a federally qualified health center (FQHC) that primarily serves a low-income Spanish-speaking community. Identification of patient-specific obstacles and misperceptions regarding COVID-19 vaccination will help primary care physicians better understand their patients and tailor interventions to improve vaccination rates in the communities that they serve. Objective: To determine the factors involved in the decision to receive the COVID-19 vaccine in a FQHC with primarily Spanish-speaking patients. Study design: Cross-sectional qualitative survey that investigates patients’ decision-making processes behind COVID-19 vaccination. Setting: Urban FQHC in Richmond, VA. Population Studied: Primarily Spanish-speaking adult immigrants 200% below federal poverty line seen by a primary care physician at Southside Health Center between January 2021 and June 2021. Instrument/intervention: Qualitative survey on factors influencing decision-making surrounding COVID-19 vaccination. Outcome Measures: The main outcome measures are the factors that motivate patients to receive the COVID-19 vaccine and the factors that prevent patients from receiving the vaccine. Anticipated Results: Approximately 200 patients participated in a phone survey. It is anticipated that the main motivations behind vaccination are to protect self, to protect loved ones, for work requirements, and out of fear of severity of disease. It is anticipated that the main hesitations are related to fear of side effects, fear of safety, and belief in low disease severity and low likelihood of getting disease. Conclusion: COVID-19 vaccination is safe and effective, but it is not universally accepted. Information gathering is crucial to improve clinician understanding of patient perception of the vaccine and to develop patient-centered interventions. This project serves as an example of a quality improvement initiative that will inform community-based vaccination interventions.
Jack Westfall
jwestfall@aafp.org 11/21/2021Great poster and abstract. Thanks for sharing at NAPCRG