SRFP097: The Complexity of Rheumatology: Patient characteristics presented during a telemedicine education program, ECHO Rheumatology
Jane Zhao, MSc; Hosna Sahak; Amanda Steiman; Claire Bombardier, MD, FRCPC
Abstract
Context
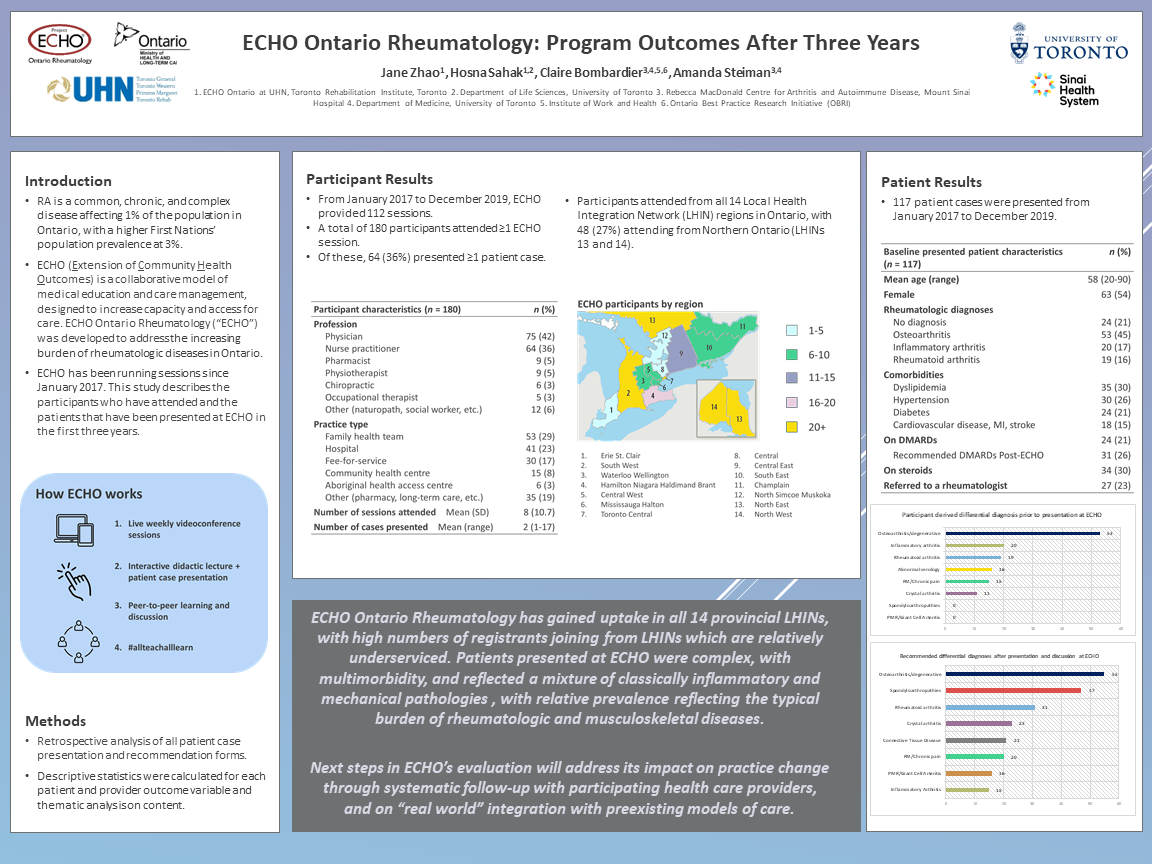
Rheumatoid Arthritis (RA) is a common, chronic, and complex disease that affects 1% of the population in Ontario, with a higher prevalence in First Nations populations at 3%. Timely and aggressive treatment of RA with disease-modifying antirheumatic drugs (DMARDs) can lead to effective management of symptoms. Left untreated, however, RA can lead to deformed joints, debilitating pain, and significantly reduced quality of life. ECHO Rheumatology (‘ECHO’) was a program developed to address the burden of RA and other rheumatic diseases in Ontario. ECHO began running weekly sessions in January 2017.
Objective
This study describes the patient characteristics and quality improvement (QI) initiatives in ECHO.
Study Design
A mixed methods study with a QI lens
Setting
ECHO (Extension for Community Healthcare Outcomes) is a collaborative model of medical education and care management, designed to increase capacity and access for care. In each weekly session, a healthcare provider (HCP) presents a patient case using a standardized patient case presentation form. Recommendations are then made from the interprofessional group and community.
Population Studied
Patient cases were summarized using the data extracted from HCPs’ weekly case presentation forms. QI opportunities were also identified from provider- and patient-level data.
Outcome Measures
1) Descriptive characteristics of patients presented and HCP participants
2) Differential diagnoses and recommendations following ECHO patient presentation
Results
From January 2017 to December 2019, ECHO provided 112 sessions with a total of 117 patient cases presented. 180 HCPs attended at least one session and 64 (36%) presented at least one case. At baseline, 63 (54%) of patients were female and mean age was 58 (range = 20-80). 24 (21%) patients had no diagnosis at baseline and 24 (21%) were on DMARDs. 27 (23%) were referred to a rheumatologist after presentation.
Conclusions
ECHO Ontario Rheumatology has gained uptake across Ontario. Patients presented at ECHO were complex, with multimorbidity, and reflected a mixture of classically inflammatory and mechanical pathologies mechanical pathologies, with relative prevalence reflecting the typical burden of rheumatologic and musculoskeletal diseases.
Next steps in ECHO’s evaluation will address its impact on practice change through systematic follow up with participating health care providers, and on “real world” integration with preexisting models of care.
Rheumatoid Arthritis (RA) is a common, chronic, and complex disease that affects 1% of the population in Ontario, with a higher prevalence in First Nations populations at 3%. Timely and aggressive treatment of RA with disease-modifying antirheumatic drugs (DMARDs) can lead to effective management of symptoms. Left untreated, however, RA can lead to deformed joints, debilitating pain, and significantly reduced quality of life. ECHO Rheumatology (‘ECHO’) was a program developed to address the burden of RA and other rheumatic diseases in Ontario. ECHO began running weekly sessions in January 2017.
Objective
This study describes the patient characteristics and quality improvement (QI) initiatives in ECHO.
Study Design
A mixed methods study with a QI lens
Setting
ECHO (Extension for Community Healthcare Outcomes) is a collaborative model of medical education and care management, designed to increase capacity and access for care. In each weekly session, a healthcare provider (HCP) presents a patient case using a standardized patient case presentation form. Recommendations are then made from the interprofessional group and community.
Population Studied
Patient cases were summarized using the data extracted from HCPs’ weekly case presentation forms. QI opportunities were also identified from provider- and patient-level data.
Outcome Measures
1) Descriptive characteristics of patients presented and HCP participants
2) Differential diagnoses and recommendations following ECHO patient presentation
Results
From January 2017 to December 2019, ECHO provided 112 sessions with a total of 117 patient cases presented. 180 HCPs attended at least one session and 64 (36%) presented at least one case. At baseline, 63 (54%) of patients were female and mean age was 58 (range = 20-80). 24 (21%) patients had no diagnosis at baseline and 24 (21%) were on DMARDs. 27 (23%) were referred to a rheumatologist after presentation.
Conclusions
ECHO Ontario Rheumatology has gained uptake across Ontario. Patients presented at ECHO were complex, with multimorbidity, and reflected a mixture of classically inflammatory and mechanical pathologies mechanical pathologies, with relative prevalence reflecting the typical burden of rheumatologic and musculoskeletal diseases.
Next steps in ECHO’s evaluation will address its impact on practice change through systematic follow up with participating health care providers, and on “real world” integration with preexisting models of care.
Jack Westfall
jwestfall@aafp.org 11/21/2021Great poster and abstract. Thanks for sharing at NAPCRG