SRFP048: From preparation to practice: impact of training on intention to practice obstetrics among family medicine residents
Jessica Yi, DO; Tyler Barreto, MD, MPH
Abstract
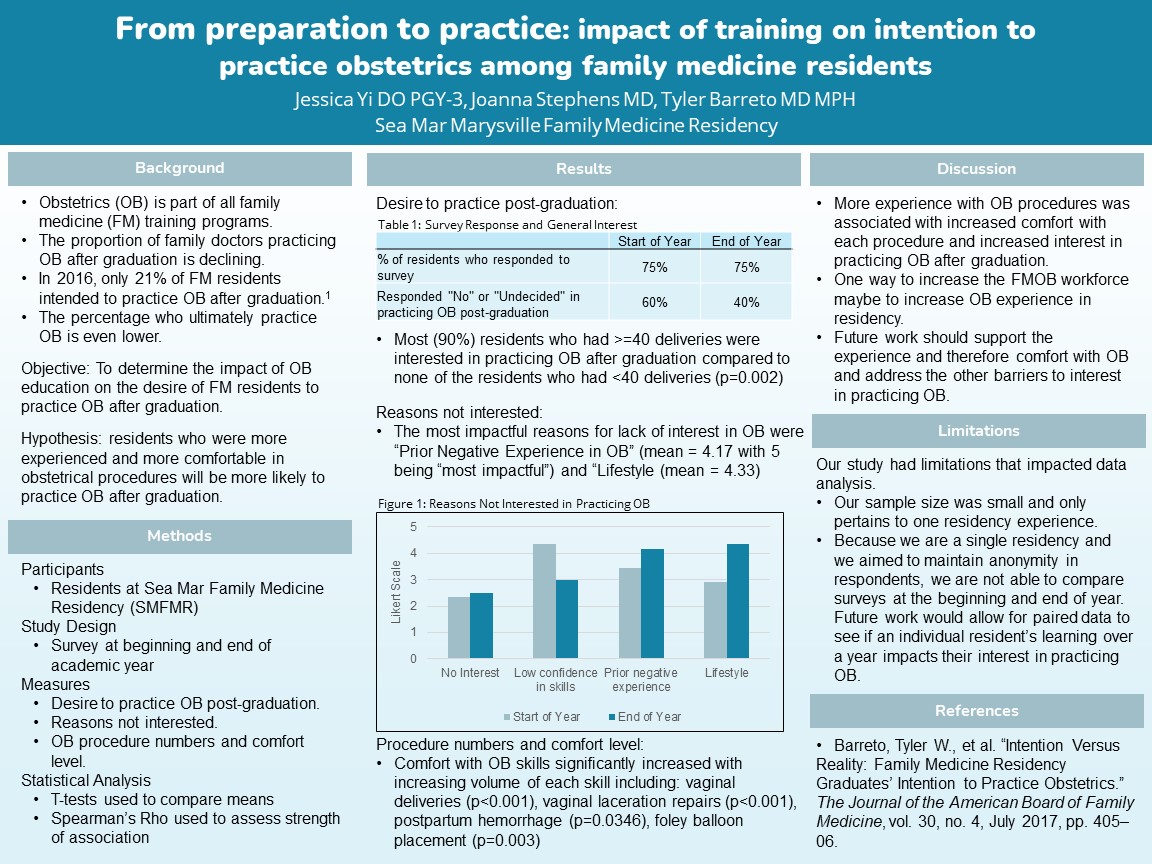
Context: Obstetrics (OB) is part of all family medicine (FM) training, and yet the proportion of family doctors practicing OB after graduation is declining. In 2016, only 23 percent of FM residents intended to practice OB after graduation. The percentage who ultimately practice OB is even lower. Objective: This study intended to determine the impact of OB education and experience on the desire of FM residents to practice OB after graduation. Investigators hypothesized that residents who were more experienced and more comfortable in obstetrical procedures would be more likely to practice OB after graduation. Study Design: A pre and post survey was developed and administered at the beginning and end of the academic year to determine changed perspectives on the desire to practice OB post-graduation. The survey included questions on OB procedure numbers and comfort and Likert scale questions on reasons for disinterest in practicing OB after graduation. Setting: A single FM residency located in a suburban Federally Qualified Health Center. Population Studied: All residents at Sea Mar Family Medicine Residency (n=20). Results: Seventy-five percent of residents responded to each survey. At the beginning of the year, 60% responded “No” or “Undecided” in their interest in OB after graduation, and 40% responded “No” or “Undecided” at the end of the year. Most (90%) residents who had >=40 deliveries were interested in practicing OB after graduation compared to none of the residents who had <40 deliveries (p=0.002). Interestingly, “Lack of confidence in OB skills” was not an impactful reason for not being interested in OB. The most impactful reasons for lack of interest in OB were “Prior negative experience in OB” (mean = 4.17 with 5 being “most impactful”) and “Lifestyle” (mean = 4.33). Interest in OB differed significantly by year in residency in that more upper levels were interested in OB. Comfort with OB skills significantly increased with increasing volume of each skill including: vaginal deliveries (p<0.001), vaginal laceration repairs (p<0.001), postpartum hemorrhage management (p=0.0346), and foley balloon placement (p=0.003). Conclusion: In a single residency, more experience with OB procedures was associated with increased comfort with each procedure and increased interest in practicing OB after graduation. Future work should support the experience and therefore comfort with OB and address the other barriers to interest in practicing OB.
Jack Westfall
jwestfall@aafp.org 11/21/2021Terrific research and poster. hoping we might change the language to maternity care, prenatal, delivery, post-partum, rather than family physicians practicing obstetrics. Because family medicine is such a large specialty with nearly 4 times as many family physicians as their are Ob/Gyns, the percent may be less important than the number. Your work is crucial to helping understand the efforts necessary to ensure an access to maternity care for all women, everywhere. the Robert Graham Center is continuing a robust portfolio of research on maternity care and hope we can connect. give us a call or email. Nice work. thanks.