SRFP121: “We want to be heard”: Perspectives on Mental Health Care among Patients at a Federally Qualified Health Center
Marvin So, MPH; Kari Carlson, MPH
Abstract
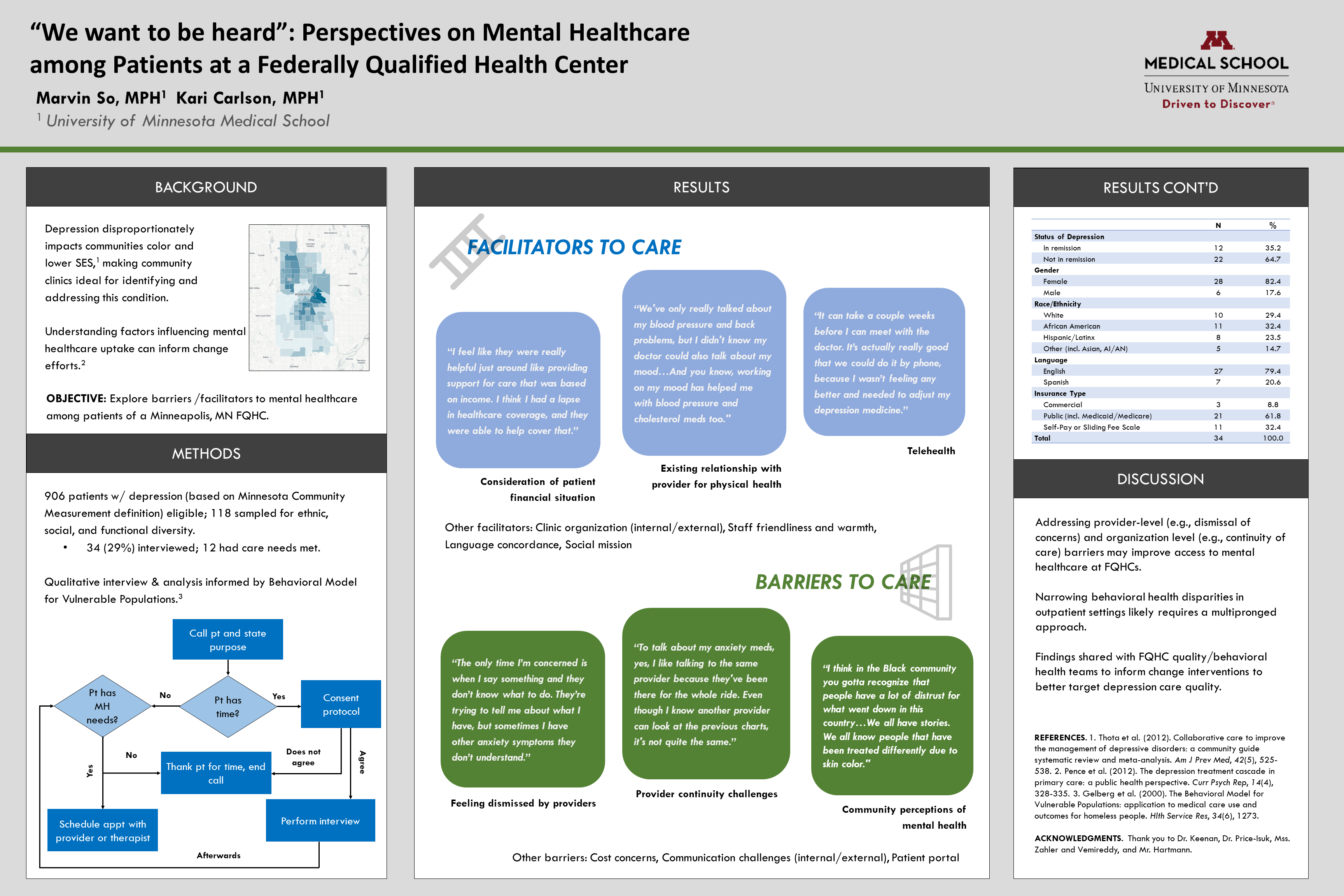
Objective: From 2020-2021, we conducted a phone-based, qualitative assessment to understand what factors hindered and helped patients diagnosed with depression at a FQHC in receiving needed mental healthcare.
Study Design: Qualitative study employing inductive (i.e., grounded theory) and deductive techniques to identify core themes.
Setting or Dataset: Patients of a single FQHC in Minneapolis with major depressive disorder or dysthymia (per ICD-10 diagnosis) were included. Patients with other mood disorders or receiving palliative care were excluded.
Population Studied: 906 FQHC patients were eligible in the overall sample, and a purposive sampling approach was used to interview 34 patients with diverse functional status, race/ethnicity, and insurance status. The analytic sample was majority non-White (32% Black, 24% Latinx, 15% Other), 20% Spanish-speaking, and 60% publicly insured.
Results: Interviews revealed multiple barriers (factors that impeded access) and facilitators (factors that enabled access) to the uptake of mental healthcare that patients encountered, from first presentation for care, initial depression diagnosis, all the way through to remission of depression symptoms. Salient barriers included feeling dismissed by providers, cost concerns, internal and external communication breakdowns, gaps in provider continuity, the patient portal, and perceptions of mental health among certain sub-populations (e.g., Black community). Salient facilitators included the clinic organization's, staff friendliness and warmth, strategies to provide care in light of patients’ financial situation, existing provider relationships for physical health needs, language concordance, the option for telehealth visits, and the clinic’s overall social mission.
Conclusion: The identified factors cast light on opportunities at multiple levels for community-based outpatient clinics to better support patients with mental health needs, and ultimately narrow persistent gaps in access.
Marvin So
so000012@umn.edu 11/18/2021Hello! Thank you for coming by to our poster. I look forward to engaging with whomever is interested and will be checking these comments periodically. if you'd like to email me directly you can do that as well (see my email listed with this comment).