SRFP118: Utilizing Primary Care to Engage Patients on Opioids in a Psychological Intervention for Chronic Pain
Sikander Chohan; Brian Ahmedani; Leah Hecht; Kirsti Autio, LMSW; Lisa Miller-Matero, PhD; Erin Tobin; Lyubov Gavrilova, BS
Abstract
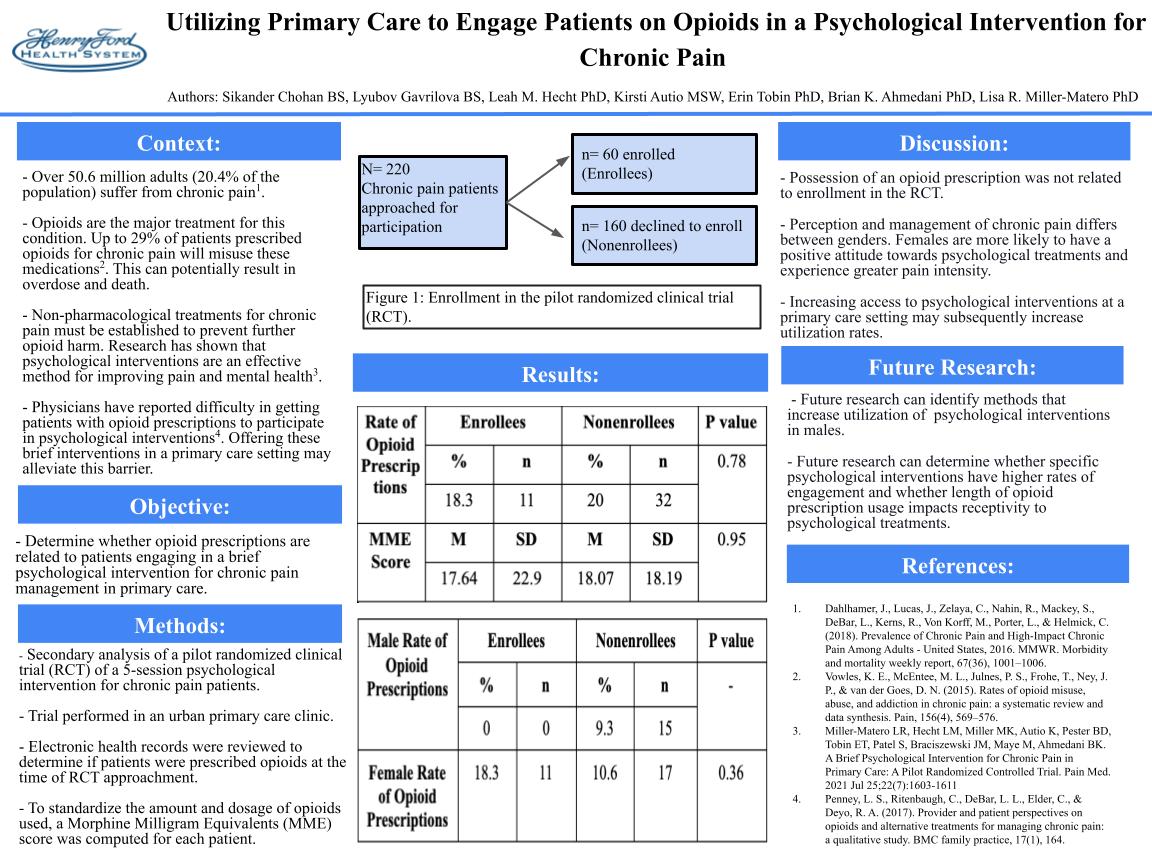
Context: Chronic pain, one of the most prevalent issues encountered in primary care, is often treated with opioid prescriptions. Overuse of these medications can cause overdose and death, creating a dire need for alternative treatment methods. Psychological interventions are effective for improving pain and distress, yet are underutilized. Physicians report difficulty engaging patients already on opioids in these interventions; it is possible that offering this intervention in a primary care setting may alleviate this barrier. Objective: Determine whether opioid prescriptions are related to patients engaging in a brief psychological intervention for chronic pain management in primary care. Study Design: Secondary analysis of a pilot randomized clinical trial of a 5-session psychological intervention for chronic pain. Setting: Primary care clinic in an urban setting Patient Population: Patients with chronic pain (N= 220) were approached to enroll in a pilot randomized clinical trial (RCT) for a brief, psychological intervention for pain in primary care. Of these, 60 participated and 160 declined. Instruments: Electronic health records were reviewed to determine whether patients were prescribed opioids or pain medications at the time they were approached about the RCT. Main outcome: Comparing opioid prescriptions in enrollees versus non-enrollees. Results: There was not a significant difference between enrollees and non-enrollees in the rate of opioid prescriptions (18.3% vs. 20%, p= .78), the morphine milligram equivalent dose of opioids (M= 17.64, SD= 22.91 vs. M= 18.07, SD= 18.19; p= .95), or the rate of non-opioid pain prescriptions (33.3% vs. 40%, p = .37). When examining for gender differences, among women, there were similar rates between enrollees and non-enrollees in the rate of opioid prescriptions (23.4% vs. 17%, p = .36). However, no males with an opioid prescription enrolled, whereas 25% of men who did not enroll had an opioid prescription. Conclusions: Among all patients, opioid prescriptions were not related to enrollment in the RCT. This suggests that engaging patients who are on opioids in a psychological treatment for chronic pain, specifically in a primary care setting, may increase utilization. However, this may be true for women, but not men. Further work needs to be done to identify methods to increase psychological intervention engagement among all patients receiving opioids, but especially men.
Jack Westfall
jwestfall@aafp.org 11/21/2021This is a great topic and research study. Nice work. Thanks