SRFP088: Relationship between maternal BMI and cesarean section procedure length in both family medicine and OB patients (Pearls)
Chanont Sricharoen, BS; Jeremy King, DO; Jenenne Geske, PhD; Birgit Khandalavala, MBBS
Abstract
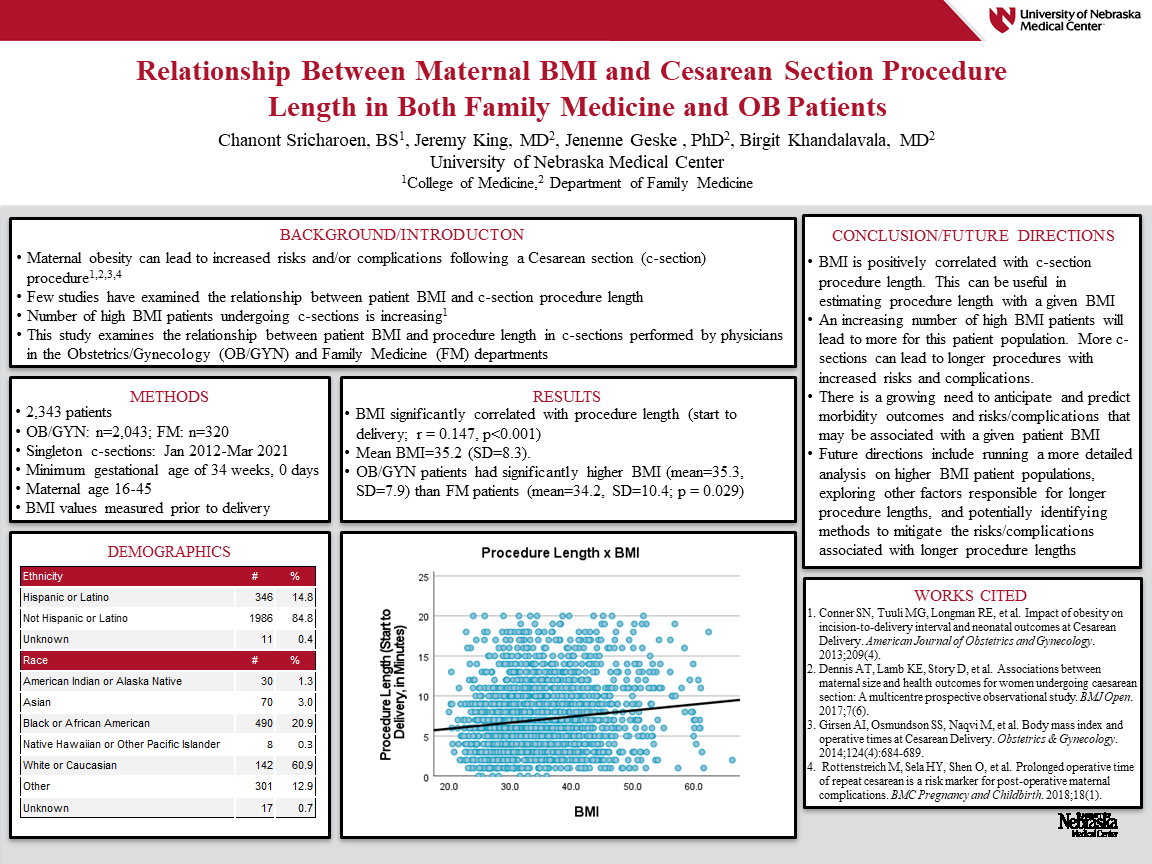
Objective – To assess the relationship between maternal BMI and procedure length in c-sections performed by family medicine and OB/GYN physicians.
Study Design – Retrospective medical records review
Setting – A midwestern regional health network
Database – Electronic Medical Records
Population Studied – 2343 patients who have undergone a c-section. Inclusion criteria include singleton deliveries by c-section in the Department of Family Medicine or the Department of Obstetrics and Gynecology who have a minimum gestational age of 34 weeks and 0 days, and maternal age of 16-45. Data include height, weight, BMI, and surgical operative time. Demographics data were also collected.
Intervention – N/A
Main Outcome Measure – length of surgical time
Results – The average BMI of patients undergoing a cesarean section was 35.2 (SD=8.3). BMI was shown to be statistically significantly correlated with procedure length (start to delivery: r=.147, p<0.001).
Conclusions – BMI is statistically significantly positively correlated with procedure length. This relationship can be useful in estimating c-section procedure length with a given BMI. With the ever-increasing number of high BMI patients seen in both Family Medicine and OB/GYN departments, more c-sections will be favored for this patient population, leading to longer procedures with increased risks and complications such as increased risk of post-operative blood transfusions, longer hospitalizations, and increased neonatal morbidity.
Jack Westfall
jwestfall@aafp.org 11/21/2021Great poster and abstract. Thanks for sharing at NAPCRG