SRFP026: Co-occurring Marijuana use among Older Adults who engage in Long-term use of Prescription Opioids
Supriya Paidemarry, BS; Summer Hoang; Tiffany Ju, BS; Carissa van den Berk-Clark, PhD, LMSW, MSW; Jennifer Bello-Kottenstette, MD, MS
Abstract
Objective: To understand factors associated with concurrent prescription opioid and marijuana use among participants over 50
Design: Secondary survey data analysis using multinomial regression
Dataset: National Survey on Drug Use and Health Data (NSDUH)
Participants: Participants in the NSDUH (N=2797) data who are over 50 and who have been using prescription opioids for at least 1 year
Outcome measures: Frequency of marijuana use (no use, casual, moderate, and consistent)
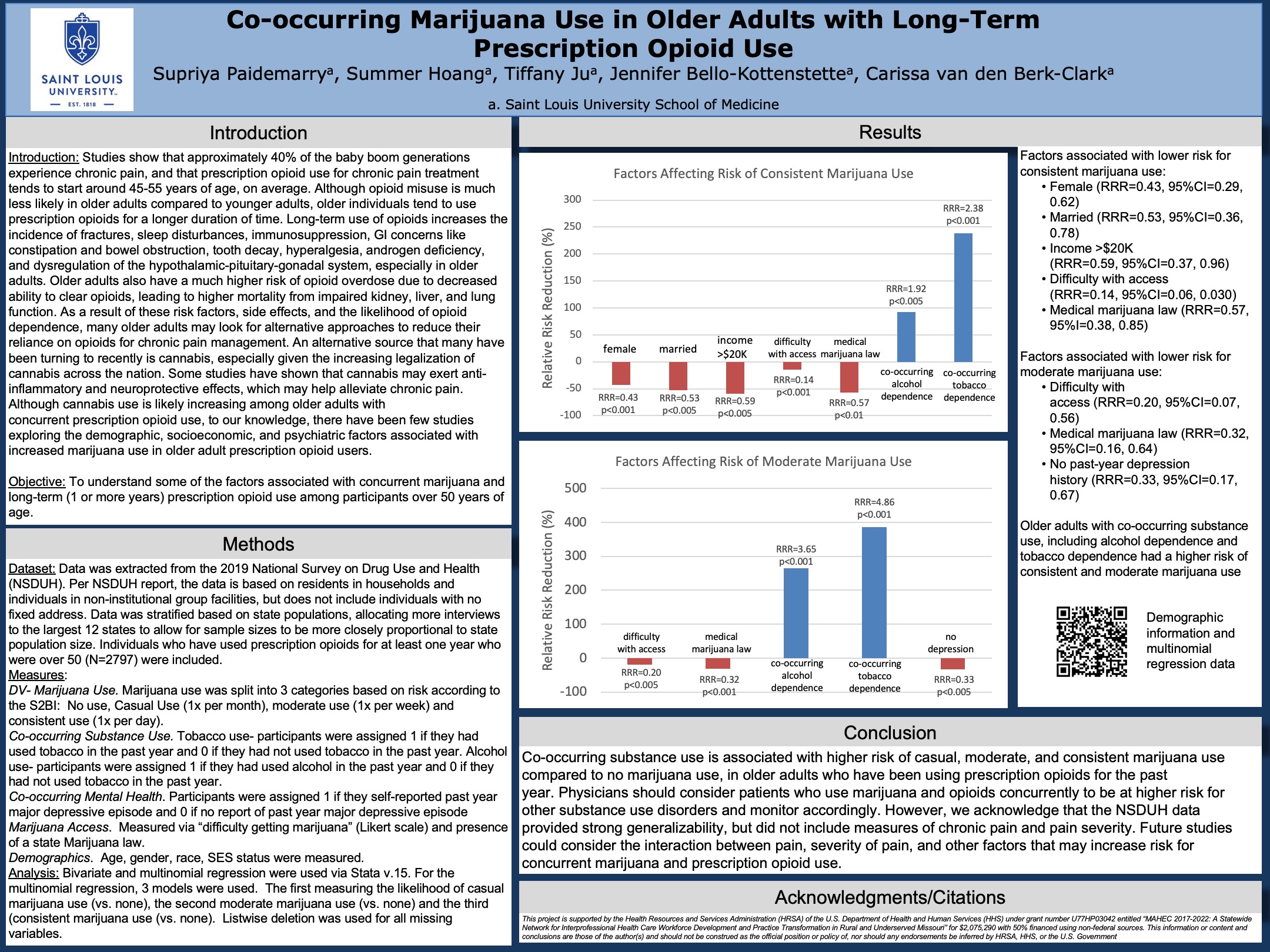
Results: Older adults who are female (RRR=0.43, 95%CI=0.29, 0.62), married (RRR=0.53, 95%CI=0.36, 078), make more than $20K (RRR=0.59, 95%CI=0.37, 0.96), find it difficult to get marijuana (RRR=0.14, 95%CI=0.062, 0.30), and live in a state with with a medical marijuana law (RRR=0.57, 95%CI= 0.38, 0.85) are at lower risk for consistent use. Older adults were at higher risk when they had co-occurring substance use issues, including alcohol dependence (RRR=1.92, 95%CI 1.27, 2.90) and tobacco dependence (RRR=2.38, 95%CI= 2.35, 4.86). Moderate and casual users had similar differences when it came to co-existing substance use issues and access to marijuana but were generally younger. Moderate users tended to have lower levels of depression (RRR=0.33, 95% CI=0.17, 0.67).
Conclusions: Co-occurring substance use is associated with higher risk of casual, moderate and consistent marijuana use compared to no marijuana use among older adults who have been using prescription opioids for the past year. Primary Care Providers should consider patients who use marijuana and opioids concurrently to be at higher risk for other substance use disorders and should monitor them carefully. Although the NSDUH data provided strong generalizability, there were no measures of chronic pain and pain severity. Future studies should consider the interaction between pain, pain severity, and other factors which increase risk for concurrent use of marijuana and prescription opioids.
Jack Westfall
jwestfall@aafp.org 11/21/2021This is a great topic and research study. Nice work. Thanks