PRP020: COVID-era Food Access
Esther Shin; Fozia Ali, MD; Olivia Chen, BS; Corina Badillo; Dirk Wristers, MD, MPH
Abstract
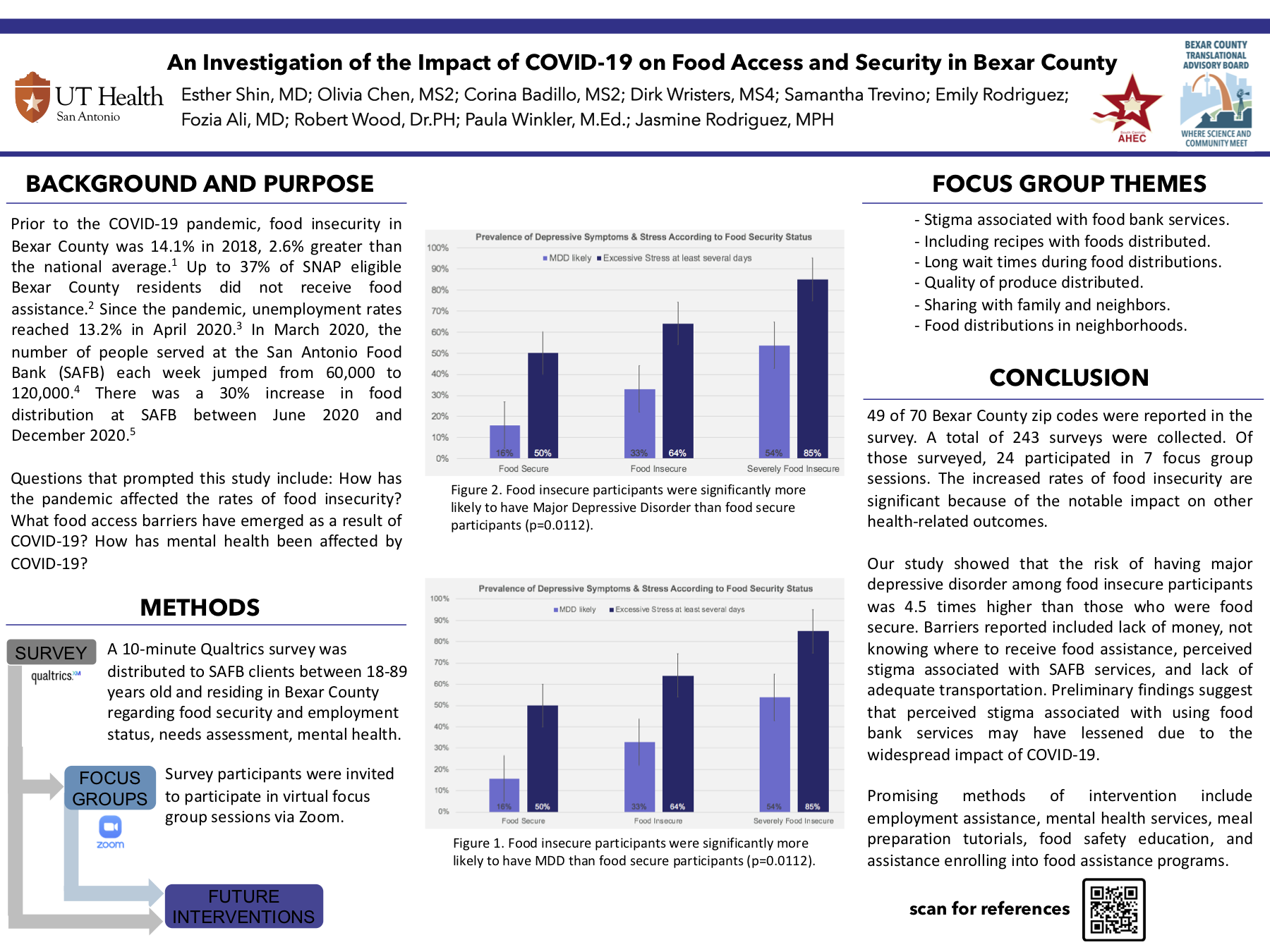
Context: Before the COVID-19 pandemic, food insecurity in Bexar County, Texas was 2.6% greater than the national average. Like much of our nation, Bexar County has seen a drastic rise in unemployment since the pandemic began. As a result, San Antonio Food Bank (SAFB) has experienced a near 100% increase in demand. Primary care physicians play an important role in bridging the gap and providing resources to combat food insecurities. Objective: The main purpose of this study was to evaluate how rates of food insecurity have been affected by COVID-19 in Bexar County, the collateral effects of food insecurity, and to determine how to better serve those affected. Study Design: Our study design utilized a mixed methods approach, in which quantitative data analysis drove qualitative data collection. First, quantitative data was collected using a 10-minute online survey developed in consultation with the Bexar County Translational Advisory Board. Then, survey participants were invited to focus group sessions via Zoom. Dataset: The survey was distributed to SAFB clients, ages 18-89, living in Bexar County. Population studied and Intervention: A total of 243 surveys were collected. Of those surveyed, 24 participants were interviewed in 7 focus group sessions. Topics discussed during these sessions included the effects of food insecurities on mental health, societal stigma associated with food insecurity, and SAFB-specific areas of improvement. Outcome Measures: The increased rates of food insecurity are significant because of the notable impact on other health-related outcomes. Results: Our study showed that the risk of having major depressive disorder among food insecure participants was 4.5 times higher than those who were food secure. Barriers reported by participants include: lack of money, not knowing where to receive food assistance, medical expenses, perceived stigma associated with SAFB services, and lack of adequate transportation - all of which contribute to an increased risk of MDD. Conclusions: Preliminary findings suggest that perceived stigma associated with using food bank services may have lessened due to the widespread impact of COVID-19. Some promising methods of intervention include employment assistance, mental health services, meal preparation tutorials, food safety education, and assistance enrolling into food assistance programs such as SNAP.
Jack Westfall
jwestfall@aafp.org 11/21/2021Terrific project. Great poster and abstract. Thanks for sharing at NAPCRG