PRP055: Metabolic Syndrome Monitoring for Patients on Antipsychotic Medications
Kurtis Morrish, MD, MPH, MSc
Abstract
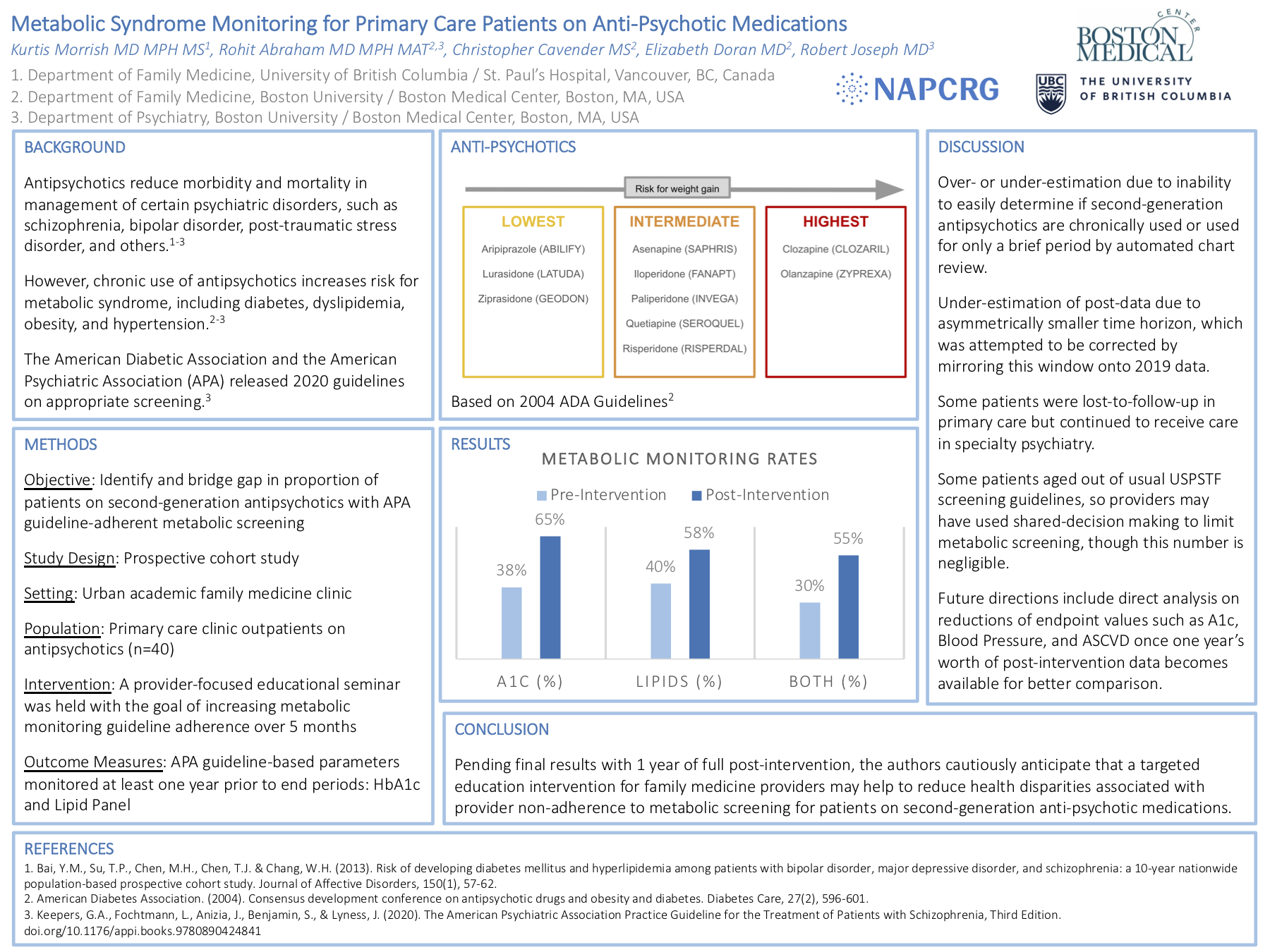
Context: Antipsychotic medications reduce morbidity and mortality in the outpatient management of certain chronic psychiatric disorders including schizophrenia, bipolar disorder, post-traumatic stress disorder, insomnia, and others. However, chronic use of antipsychotic medications introduces risk for many side effects, notably weight gain, insulin resistance, dyslipidemia, hypertension, and metabolic syndrome. In 2004, the American Diabetic Association and the American Psychiatric Association (APA) collaborated to release guidelines detailing an appropriate method for screening for metabolic syndrome in patients on antipsychotic medications. These guidelines were updated and streamlined in 2020 by the APA. Despite the importance of screening for metabolic syndrome in patients taking antipsychotic medication, provider adherence to guideline recommendations remains as low as 20-30% in the primary care setting. Objective: Increase the proportion of patients on antipsychotic medications receiving 2020 guideline-adherent metabolic monitoring screening. Study Design: Prospective cohort study. Setting: Urban multi-provider family medicine clinic setting. Population Studied: Primary care outpatients (n=211) on chronic antipsychotics. Intervention: After an initial retrospective chart review from the 2019 calendar year, a provider-focused educational seminar was held on March 2021 with the goal of increasing metabolic monitoring guideline adherence over 6 months. Outcome Measure: Provider adherence to guideline-based parameters monitored on at least a yearly basis: blood pressure, basal metabolic index, lipid panel, and A1c. Results: Guideline-adherent screening rates in this population were as low as 33%. Guideline adherence in patients for whom psychiatry ordered their medications was found to be 56%, while patients for whom family medicine ordered their medications were appropriately screened 20% of the time. Further results continue to be pending, including comparison to the 6-month interval of time after the provider-focused educational seminar. Conclusion: Patients on chronic antipsychotics managed by family medicine providers tended to have a far lower rate of APA-recommended metabolic monitoring as compared to patients managed by psychiatry providers. Pending final results, the authors anticipate that a targeted education intervention for family medicine providers may or may not help to reduce these health disparities.
Len Finn
leonard.finn@gmail.com 11/20/2021please see our posters on mindful eating and healthy nutrition, #55 and #56, would you and your patients be interested in participating in such a group visit intervention sometime in the future?