PRP092: Transdisciplinary, Multi-Institutional Team Research During COVID-19
Mary Alice Scott, PhD; Ronan Cox, BA; Sashiel Pina, MA; Rachel Ceballos; Justin Falls; Olivia Stuertz, BA
Abstract
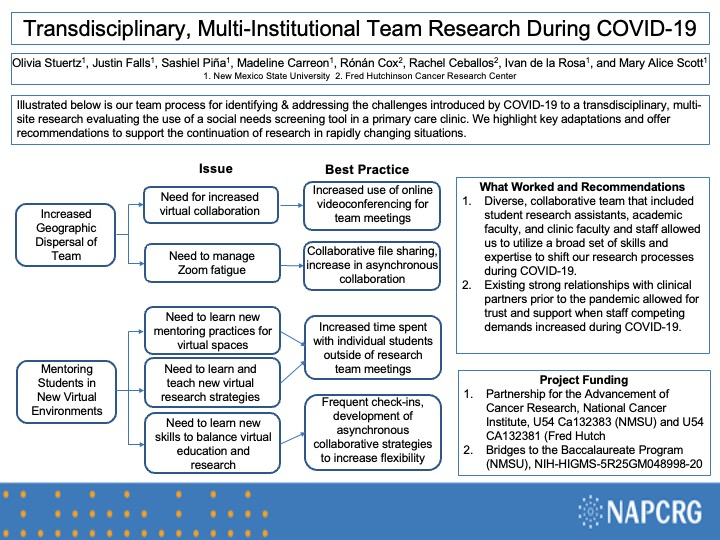
Context: Social needs screening tools can improve patient care quality. Many clinics have integrated these tools into their intake process in recent years. However, assessing tool efficacy is challenging, as it requires intensive research. Assessment in a clinical setting is even more challenging during public health crises such as COVID-19. Our research team navigated the complexities of integrating research process into clinical workflows during the current global pandemic to conduct a study examining the use of a social needs screening tool in a U.S.-Mexico border region primary health care setting. The lessons learned from our study can help guide future research in family medicine and primary care.
Objective: How can team science help a transdisciplinary, multi-institutional team successfully conduct research in and for a primary health care setting?
How did our team structure and process enable us to adapt to the challenges of the COVID-19 pandemic?
Study Design: Description of process of team development and strategies to address challenges
Setting: collaborative project among a minority-serving, land-grant institution in the U.S. southwest, a cancer center in the Pacific Northwest, and a primary care clinic serving underserved, rural to semi-urban communities in the U.S.-Mexico border region.
Population studied: process focuses on the research team that implemented the study, including an anthropologist, social worker, public health sciences faculty and staff, students, primary care clinic administrators and staff
Intervention/instrument: Transdisciplinary team science
Outcome measures: none
Results: Our team maintained a strong relationship with the clinic staff throughout an ongoing public health crisis. Communication was key to developing a path forward with this study, as they were able to observe and communicate information on how patients from a medically underserved, predominantly Latina/o community with limited access to home computers, smart phones, and internet were able to access care when in-person visits were limited. Through the adaptation of this pilot project to a fully remote intervention, we developed workflows and study documents for in-person and remote recruitment and consenting of participants that may be used as models for future studies operating in rural environments or under various circumstances when in-person contact creates barriers to participation or is restricted due to public health guidelines.
Objective: How can team science help a transdisciplinary, multi-institutional team successfully conduct research in and for a primary health care setting?
How did our team structure and process enable us to adapt to the challenges of the COVID-19 pandemic?
Study Design: Description of process of team development and strategies to address challenges
Setting: collaborative project among a minority-serving, land-grant institution in the U.S. southwest, a cancer center in the Pacific Northwest, and a primary care clinic serving underserved, rural to semi-urban communities in the U.S.-Mexico border region.
Population studied: process focuses on the research team that implemented the study, including an anthropologist, social worker, public health sciences faculty and staff, students, primary care clinic administrators and staff
Intervention/instrument: Transdisciplinary team science
Outcome measures: none
Results: Our team maintained a strong relationship with the clinic staff throughout an ongoing public health crisis. Communication was key to developing a path forward with this study, as they were able to observe and communicate information on how patients from a medically underserved, predominantly Latina/o community with limited access to home computers, smart phones, and internet were able to access care when in-person visits were limited. Through the adaptation of this pilot project to a fully remote intervention, we developed workflows and study documents for in-person and remote recruitment and consenting of participants that may be used as models for future studies operating in rural environments or under various circumstances when in-person contact creates barriers to participation or is restricted due to public health guidelines.
Diane Harper
harperdi@med.umich.edu 11/21/2021thank you for sharing with NAPCRG. Great that you have NIH support!