PRP076: Service Co-design with Older People who have Homeless Histories – Early Lessons from a Work in Progress
Lara Nixon, MD, FCFP, CCFP(COE), FCFP; Martina Kelly, MD, PhD, CCFP, MA, MBChB; Ashley McInnes, PhD; Megan Sampson, MA
Abstract
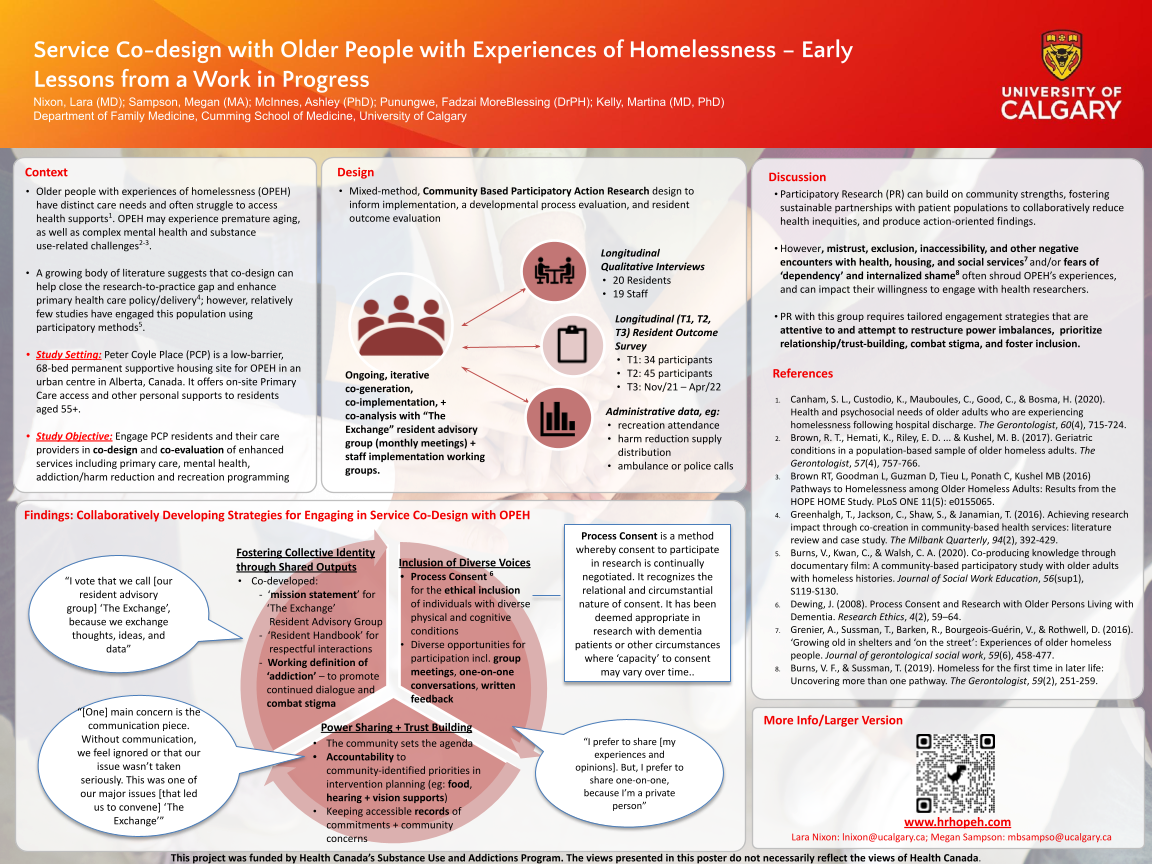
Context: Older people with experiences of homelessness have distinct care service needs and often struggle to access health supports. Patient engagement in service co-design can enhance care delivery; however, service needs are currently under-explored, with few studies engaging this population using participatory methods. Objective: This study aims to engage older people with homeless histories and their care providers in co-design of enhanced care supports including primary care, mental health, addiction and recreation programming in permanent supportive living committed to harm reduction policy. Design: mixed-method, Participatory Action Research; qualitative data collection including: (a) ‘townhall meetings’, open to all residents and staff, for broad idea generation; (b) a designated Community Advisory Group (CAG) “The Exchange”, contributing to intervention co-design; (c) waves of interviews with residents and staff, and staff-specific focus groups to identify early implementation barriers/facilitators. Thematic analyses has been iterative with member checking. Setting: 68-bed supportive living facility in a Canadian large urban centre, providing primary health and personal supports for men and women aged 55+, unable to secure housing elsewhere and with ongoing substance use challenges. Participants as of May 2021: 7 residents, 10 staff participants over 16 CAG meetings; 10 residents, 18 staff in interviews. Findings: Tensions surrounding power dynamics and organizational culture were identified as implementation barriers. Community co-developed strategies to address these include: (i) engaging flexibly, with multiple opportunities for individual and group sharing, to include diverse voices and promote power sharing; and (ii) co-designing educational opportunities to mitigate stigma around substance use and social determinants of health. ‘Process consent’, where ‘informed consent’ is continuously revisited, has helped facilitate ethical inclusion of residents with ranging physical and cognitive capacities. Preliminary conclusions: Intentional sharing of power and flexible approaches are essential to engaging older people with homeless histories, and their care providers, in co-designing services relevant to their needs and community-driven care.
Diane Harper
harperdi@med.umich.edu 11/21/2021WOW! This is an amazing example of participatory research. Please continue to update us at NAPCRG on your projects and results!