PRP067: Prototype of a Harmonized Healthcare Database across Institutions
Kimberly Fulda, DrPH; Usha Sambamoorthi; David Schneider, MD, MSPH; Sravan Mattevada, MS; Imam Xierali, PhD; Anna Espinoza, MD; Omair Muzaffar, MPH; Melissa Acosta, PhD; Richard Young, MD; Somer Blair, PhD; Chance Strenth, PhD; Leo Gonzalez, MA; Sydney Manning
Abstract
Context: The need for data harmonization extracted from Electronic Health Records (EHR) is rapidly growing as the health systems and clinicians use different EHR systems. Often, the computer systems or software are used for administration, billing, and clinical documentation. The different EHR systems cannot exchange information that can be readily and meaningfully used for research.
Objective: The purpose of this study is to describe the process of data harmonization for research using EHR data from three healthcare systems. Specifically, we describe the challenges and outline the potential solutions.
Study Design: Cross-sectional, cohort, case-control or longitudinal study designs can be used.
Setting or Dataset: Harmonized electronic health records used in primary care of three healthcare systems.
Population studied: All adult patients seeking care in family medicine clinics at three academic medical centers in North Texas between January 1, 2019 and December 31, 2019.
Outcome Measures: Prevalence of treated chronic conditions, clinical management, and bio-markers of chronic conditions.
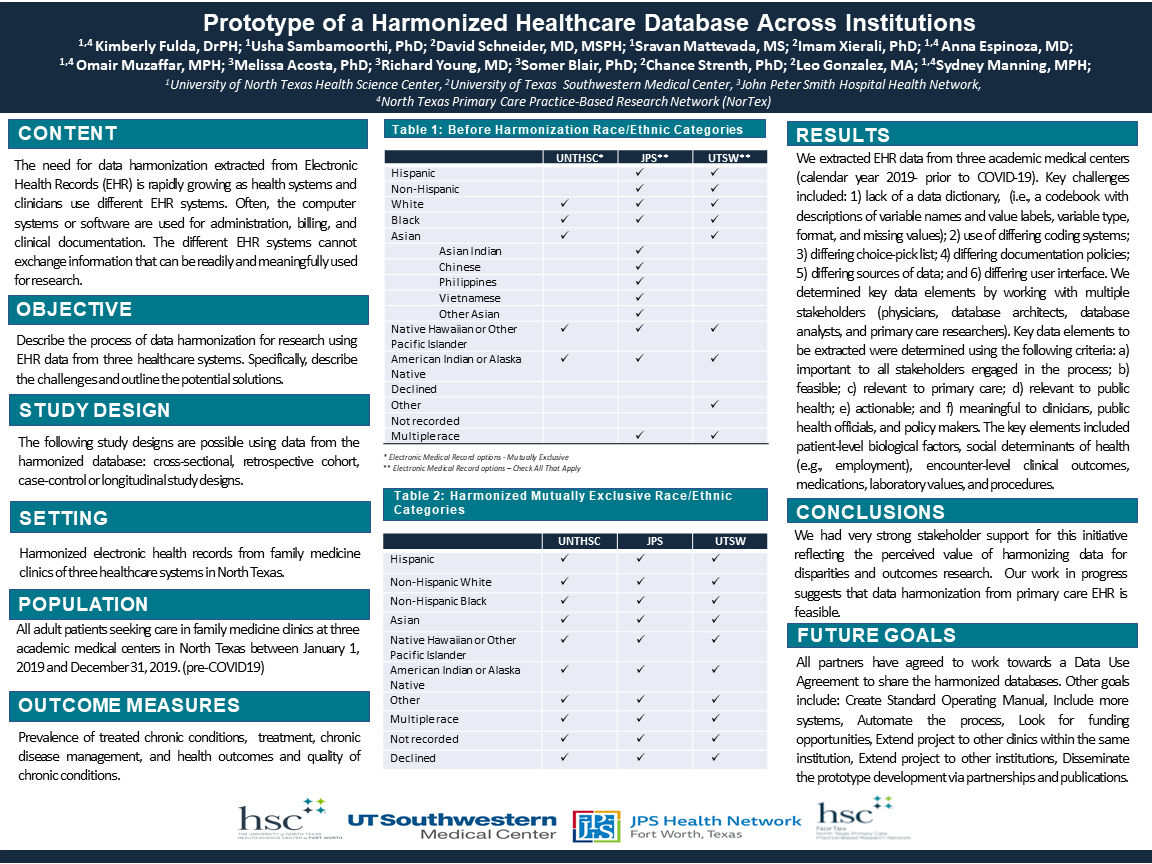
Results: We extracted EHR primary care data from three academic medical centers (calendar year 2019- prior to COVID-19). Key challenges included: 1) lack of data dictionary (i.e., a codebook with descriptions of variable names and value labels, variable type, format, and missing values); 2) use of differing coding system; 3) differing choice-pick list; 4) differing documentation policies; 5) differing sources of data; and 6) differing user interface. We determined key data elements by working with multiple stakeholders (physicians, database architects, database analysts, and primary care researchers). Key data elements to be extracted were determined using the following criteria: a) important to all stakeholders engaged in the process; b) feasible; c) relevant to primary care; d) relevant to public health; e) actionable; and f) meaningful to clinicians, public health officials, and policy makers. The key elements included patient-level biological factors, social determinants of health (e.g., employment), encounter-level clinical outcomes, medications, laboratory values, and procedures.
Conclusion: There was very strong stakeholder support for this initiative reflecting the perceived value of harmonizing data for disparities and outcomes research. Our work in progress suggests that data harmonization from primary care EHR is feasible.
Objective: The purpose of this study is to describe the process of data harmonization for research using EHR data from three healthcare systems. Specifically, we describe the challenges and outline the potential solutions.
Study Design: Cross-sectional, cohort, case-control or longitudinal study designs can be used.
Setting or Dataset: Harmonized electronic health records used in primary care of three healthcare systems.
Population studied: All adult patients seeking care in family medicine clinics at three academic medical centers in North Texas between January 1, 2019 and December 31, 2019.
Outcome Measures: Prevalence of treated chronic conditions, clinical management, and bio-markers of chronic conditions.
Results: We extracted EHR primary care data from three academic medical centers (calendar year 2019- prior to COVID-19). Key challenges included: 1) lack of data dictionary (i.e., a codebook with descriptions of variable names and value labels, variable type, format, and missing values); 2) use of differing coding system; 3) differing choice-pick list; 4) differing documentation policies; 5) differing sources of data; and 6) differing user interface. We determined key data elements by working with multiple stakeholders (physicians, database architects, database analysts, and primary care researchers). Key data elements to be extracted were determined using the following criteria: a) important to all stakeholders engaged in the process; b) feasible; c) relevant to primary care; d) relevant to public health; e) actionable; and f) meaningful to clinicians, public health officials, and policy makers. The key elements included patient-level biological factors, social determinants of health (e.g., employment), encounter-level clinical outcomes, medications, laboratory values, and procedures.
Conclusion: There was very strong stakeholder support for this initiative reflecting the perceived value of harmonizing data for disparities and outcomes research. Our work in progress suggests that data harmonization from primary care EHR is feasible.
Diane Harper
harperdi@med.umich.edu 11/21/2021OUTSTANDING!! Standardization across health systems is possible! Thank you for sharing with us at NAPCRG.