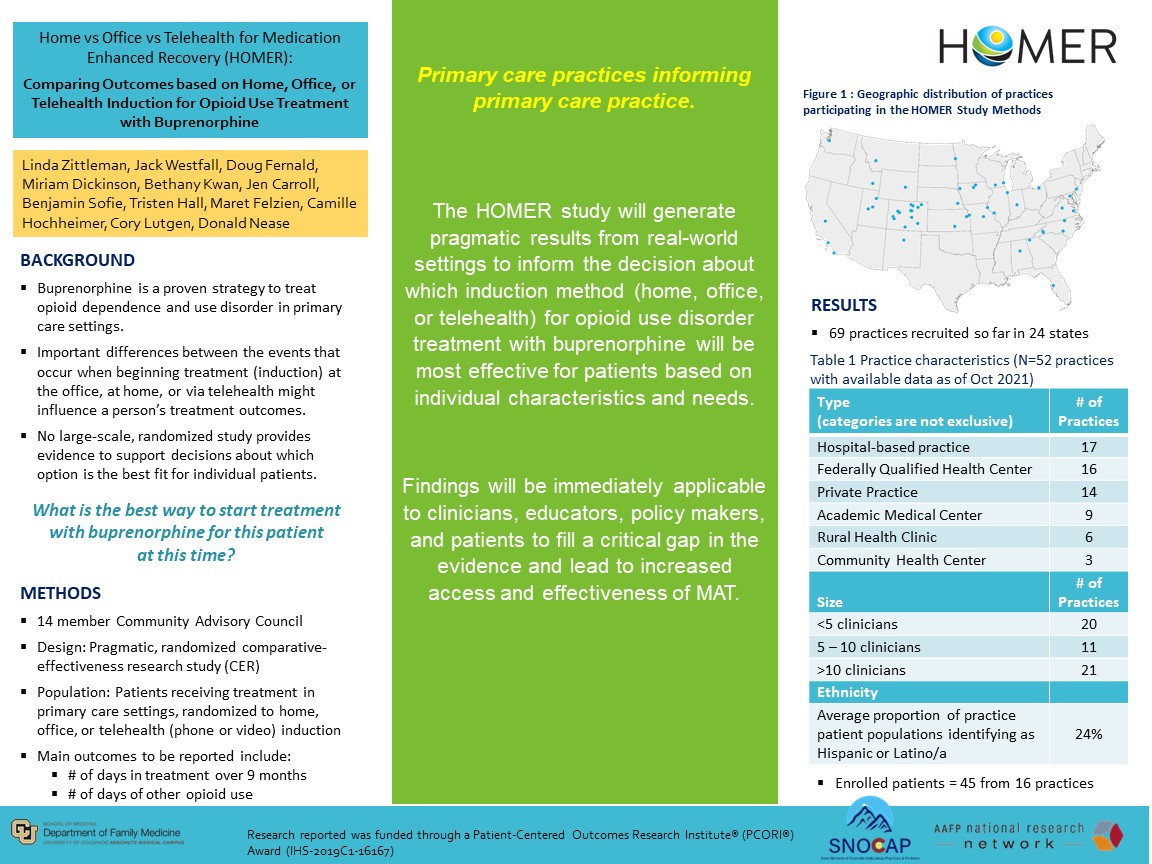
PRP017: Comparing Outcomes based on Home, Office, or Telehealth Induction for Opioid Use Treatment with Buprenorphine
Linda Zittleman, MSPH; John Westfall, MD, MPH; Camille Hochheimer, PhD; L. Miriam Dickinson, PhD; Donald Nease, MD; Cory Lutgen, BS, BSc; Douglas Fernald, MA; Ben Sofie, MSW; Jennifer Carroll, MD, MPH; Bethany Kwan, PhD, MSPH; Maret Felzien, MA
Jack Westfall
jwestfall@aafp.org 11/21/2021This is a very important topic and research study. Nice work. Thanks