PRP075: Role of telemedicine in the care of persons living with dementia and their caregivers in urban and rural regions of Canada
Vladimir Khanassov, MD, MSc; Geneviève Arsenault-Lapierre, PhD; Isabelle Vedel, MD, PhD
Abstract
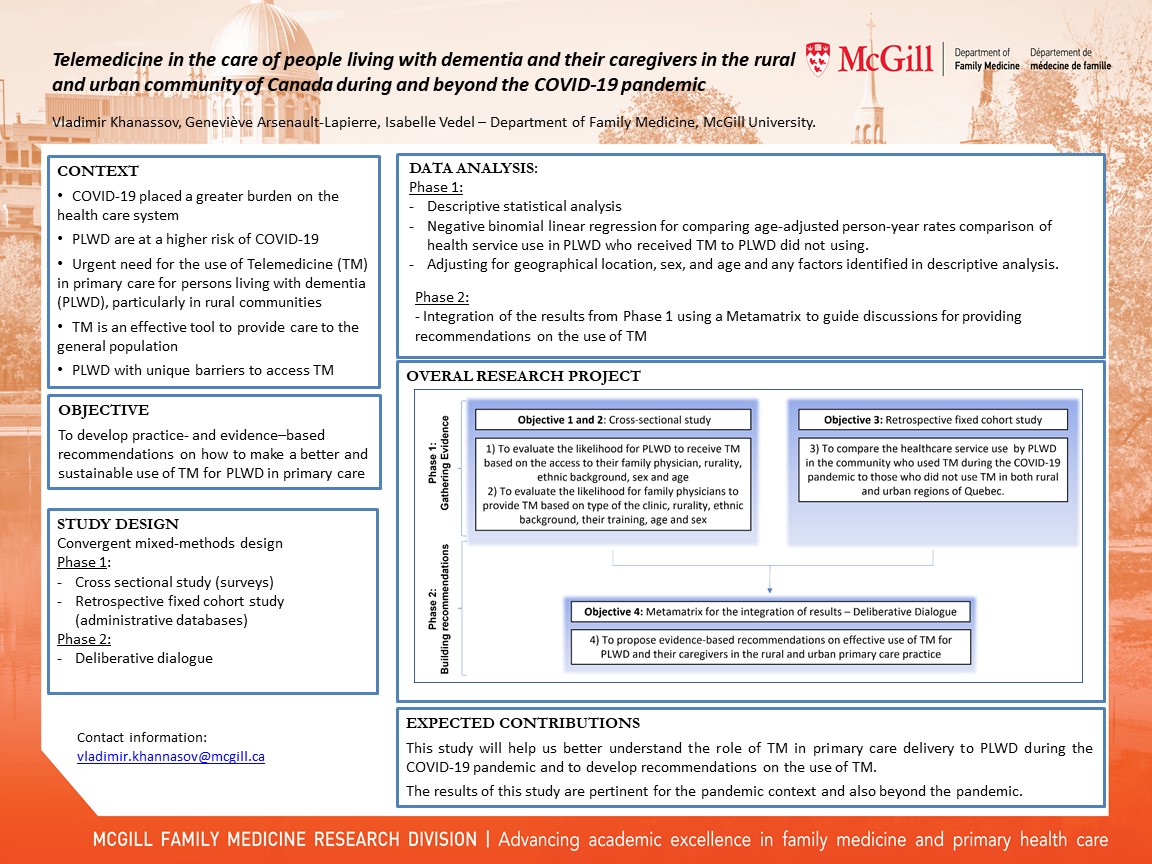
Context: There is an urgent need to improve the use of telemedicine (TM) by primary care clinicians for persons living with dementia (PWD), particularly in rural communities. TM could alleviate geographically based disparities by improving continuity of care with a family physician which could lead to fewer avoidable hospitalizations. However, the use of TM with PWD might be challenging because of the cognitive or physical limitations.
Objective: To develop practice- and evidence–based recommendations on how to make a better and sustainable use of TM. Our project has the following research questions: 1) to compare the impact of TM on health services use by PWD and caregivers in urban and rural communities, 2) to examine the PWD, caregivers’ and the clinicians’ experiences with TM, 3) to develop practice- and evidence-based recommendations for the effective use of TM for PWD and caregivers.
Study design: a convergent mixed-method design: 1) a quasi-experimental design with historical controls to identify the impact of TM during the pandemic on health service use and mortality in PWD using health administrative databases from the provinces of Canada (QC, ON, AB, SK). Cross-sectional monthly cohorts of PWD during the pandemic (Mar 20-Feb 21) will be compared to PWD during the preceding year (Mar 19-Feb 20); 2) thematically analysed open ended questions from two surveys developed by the Alzheimer Society of Canada and the College of Family Physicians of Canada to understand the PWD, caregivers’ and the family physicians’ experiences with TM; 3) integration of the results from both studies to develop and evaluate practice- and evidence-based recommendations. The criteria of the Appraisal of Guidelines, Research and Evaluation (AGREE) tool will be used for clinical practice guideline development.
Setting: Primary care practices of the four provinces of Canada
Population: PWD 65 years old and over seen at least once via teleconsultation from March 2020 to March 2021 identified in the provincial administrative databases.
Outcomes: 1) the impact of TM will be measured from indicators of health services use (e.g., visits to family physicians (in-person, by phone or video), ED visits, hospitalizations and etc.); a list of enablers and barriers of TM use will be created from the thematically analyzed questionnaires; 3) based on the AGREE criteria the recommendations on TM use for PWD will be developed.
Objective: To develop practice- and evidence–based recommendations on how to make a better and sustainable use of TM. Our project has the following research questions: 1) to compare the impact of TM on health services use by PWD and caregivers in urban and rural communities, 2) to examine the PWD, caregivers’ and the clinicians’ experiences with TM, 3) to develop practice- and evidence-based recommendations for the effective use of TM for PWD and caregivers.
Study design: a convergent mixed-method design: 1) a quasi-experimental design with historical controls to identify the impact of TM during the pandemic on health service use and mortality in PWD using health administrative databases from the provinces of Canada (QC, ON, AB, SK). Cross-sectional monthly cohorts of PWD during the pandemic (Mar 20-Feb 21) will be compared to PWD during the preceding year (Mar 19-Feb 20); 2) thematically analysed open ended questions from two surveys developed by the Alzheimer Society of Canada and the College of Family Physicians of Canada to understand the PWD, caregivers’ and the family physicians’ experiences with TM; 3) integration of the results from both studies to develop and evaluate practice- and evidence-based recommendations. The criteria of the Appraisal of Guidelines, Research and Evaluation (AGREE) tool will be used for clinical practice guideline development.
Setting: Primary care practices of the four provinces of Canada
Population: PWD 65 years old and over seen at least once via teleconsultation from March 2020 to March 2021 identified in the provincial administrative databases.
Outcomes: 1) the impact of TM will be measured from indicators of health services use (e.g., visits to family physicians (in-person, by phone or video), ED visits, hospitalizations and etc.); a list of enablers and barriers of TM use will be created from the thematically analyzed questionnaires; 3) based on the AGREE criteria the recommendations on TM use for PWD will be developed.
Diane Harper
harperdi@med.umich.edu 11/21/2021very good work. Thank you for sharing it with NAPCRG. Please let us know your continuing results.