PRP015: Change of paradigm of primary care: telemedicine in the care of elderly population
Vladimir Khanassov, MD, MSc; Marwa Ilali; Isabelle Vedel, MD, PhD
Abstract
Context: The coronavirus pandemic has significantly changed the approach to healthcare service delivery from in person care to telemedicine. While it is an efficient way to deliver care for the general population, it is a challenge for the elderly population (e.g., access to video devices, smart phones, hearing and visual impairment, cognitive decline).
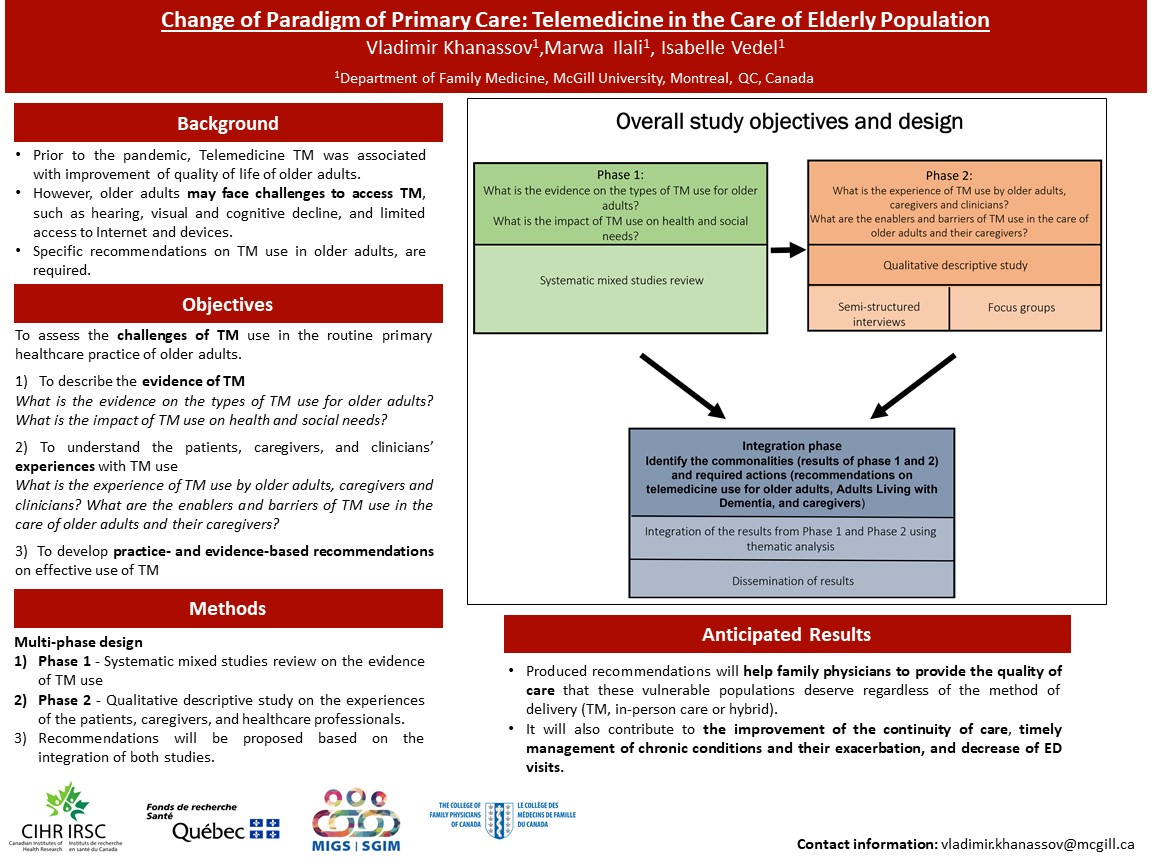
Objective: To examine the potential effect of telemedicine use on the routine primary care practice of elderly patients living in the community. Our research questions are: 1) What is the evidence of telemedicine use in the routine primary care practice of elderly patients? 2)What is the experience of telemedicine use by elderly patients, family physicians and nurses? 3) What are the barriers and facilitators of telemedicine use in the routine primary care practice of elderly patients?
Multi-phase study design: 1) a systematic review on the evidence of telemedicine use, 2) qualitative descriptive study on the experiences of the patients and healthcare professionals with the integration of the results from both phases to propose the recommendations.
Dataset: literature search of the studies in English, French or Russian listed in MEDLINE, PsycINFO, EMBASE, CINAHL, AgeLine, the Cochrane Library published before November 2020; protocol published at the PROSPERO, CRD42021237686.
Population: Elderly patients will be recruited from four McGill family medicine units (40 in total) for the individual semi-structured interviews, focus groups with the family physicians and nurses at each practice. A narrative approach to describe the existing evidence on telemedicine for elderly patients and thematic analysis for the qualitative study will be used.
Outcomes: 1) the impact on the individual outcomes (e.g., satisfaction with the care, control of the diseases, impact on social isolation, education on the disease) and system outcomes (e.g., access to primary care provider, frequency of ER visits for the conditions sensitive to primary care); 2) themes on the attitude towards TM use (e.g., convenience), barriers (e.g., technical challenges) and facilitators (e.g., decreased cost) to optimal use of TM by the patients and primary care healthcare professionals.
Objective: To examine the potential effect of telemedicine use on the routine primary care practice of elderly patients living in the community. Our research questions are: 1) What is the evidence of telemedicine use in the routine primary care practice of elderly patients? 2)What is the experience of telemedicine use by elderly patients, family physicians and nurses? 3) What are the barriers and facilitators of telemedicine use in the routine primary care practice of elderly patients?
Multi-phase study design: 1) a systematic review on the evidence of telemedicine use, 2) qualitative descriptive study on the experiences of the patients and healthcare professionals with the integration of the results from both phases to propose the recommendations.
Dataset: literature search of the studies in English, French or Russian listed in MEDLINE, PsycINFO, EMBASE, CINAHL, AgeLine, the Cochrane Library published before November 2020; protocol published at the PROSPERO, CRD42021237686.
Population: Elderly patients will be recruited from four McGill family medicine units (40 in total) for the individual semi-structured interviews, focus groups with the family physicians and nurses at each practice. A narrative approach to describe the existing evidence on telemedicine for elderly patients and thematic analysis for the qualitative study will be used.
Outcomes: 1) the impact on the individual outcomes (e.g., satisfaction with the care, control of the diseases, impact on social isolation, education on the disease) and system outcomes (e.g., access to primary care provider, frequency of ER visits for the conditions sensitive to primary care); 2) themes on the attitude towards TM use (e.g., convenience), barriers (e.g., technical challenges) and facilitators (e.g., decreased cost) to optimal use of TM by the patients and primary care healthcare professionals.
Jack Westfall
jwestfall@aafp.org 11/21/2021Terrific project. Great poster and abstract. Thanks for sharing at NAPCRG