PRP086: The association between sleep disruption and depression in patients with 30 to 90 day opioid analgesic use
Sathwik Booreddy, BS; Lisa Miller-Matero, PhD; Joanne Salas, MPH; Jeffrey Scherrer, PhD
Abstract
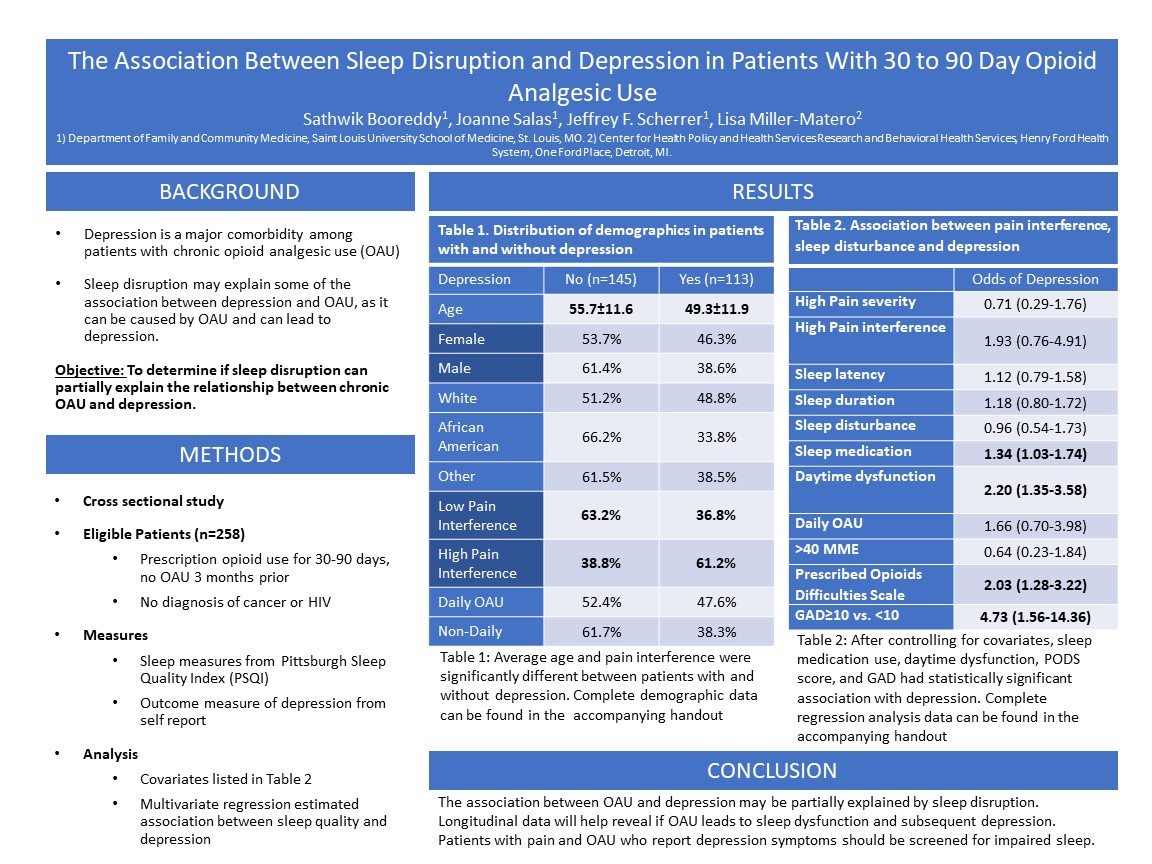
Context: Depression is a major comorbidity among patients with chronic opioid analgesic use (OAU). OAU has a bi-directional relationship with depression. The mechanisms of this relationship remain poorly understood. Not all patients with OAU have comorbid depression, suggesting that other factors may mediate this relationship. Objective: Determine whether sleep disruption partly explains the association between chronic OAU and depression. Study Design: Cross-sectional. Settings/Data set: Patients starting a new period of 30 to 90 day opioid use were invited to a longitudinal study of pain, OAU and depression. Data collected with standardized, validated instruments via web based self-administration or via phone interview. Population studied: Eligible patients (n=258) had prescription opioid use for 30-90 days, no OAU for 3 months prior to this new episode of use, no diagnosis of cancer or HIV, and had completed the baseline assessment. Outcome measure: Depression. Results: Patients without depression were on average 49.3 (SD±11.9) years of age, 46.3% female, and 48.8% white race. Patients who did not experience depression were on average 55.7 (SD±11.6) years of age, 53.7% female, and 51.2% white race. All measures of sleep disruption differed significantly between patients with and without depression (p<0.001). Among those with depression, average sleep latency was 2.07 (SD±1.10), sleep duration of 1.64 (SD±1.03), sleep disturbance of 13.2 (SD±5.09), sleep medication of 1.75 (SD±1.41), and sleep related daytime dysfunction of 1.41 (SD±0.93). Patients who did not have depression had an average sleep latency of 1.33 (SD±1.11), sleep duration of 1.08 (SD±0.97), sleep disturbance of 9.73 (SD±4.74), sleep medication of 1.17 (SD±1.39), and sleep related daytime dysfunction of 0.62 (SD±0.71). Both sleep medication (OR=1.26, 95%CI:1.01-1.57) and sleep related daytime dysfunction (OR=2.37, 95%CI:1.58-3.56) showed positive associations with depression. When controlling for frequency and dose of prescription opioids and for comorbid generalized anxiety disorder, sleep medication use and sleep related daytime dysfunction retained their significant association with depression. Conclusions: The association between OAU and depression may be partially explained by sleep disruption. Longitudinal data will help reveal if OAU leads to sleep dysfunction and subsequent depression. Patients with pain and OAU who report depression symptoms should be screened for impaired sleep.
Diane Harper
harperdi@med.umich.edu 11/21/2021It is wonderful to see the collaborations between institutions to tackle the issue of OAU and depression. Thank you for sharing it with NAPCRG.