PRP031: Enhanced Care Planning Study: Patient Health Risks, Priorities, and Assistance Preferences
Kristen O'Loughlin, MA, MS; Jacqueline Britz, MD, MSc; Jennifer Hinesley, PsyD; Alex Krist, MD, MPH; Roy Sabo, PhD; Benjamin Webel, BA; Paulette Lail Kashiri, MPH; Alicia Richards, BS
Abstract
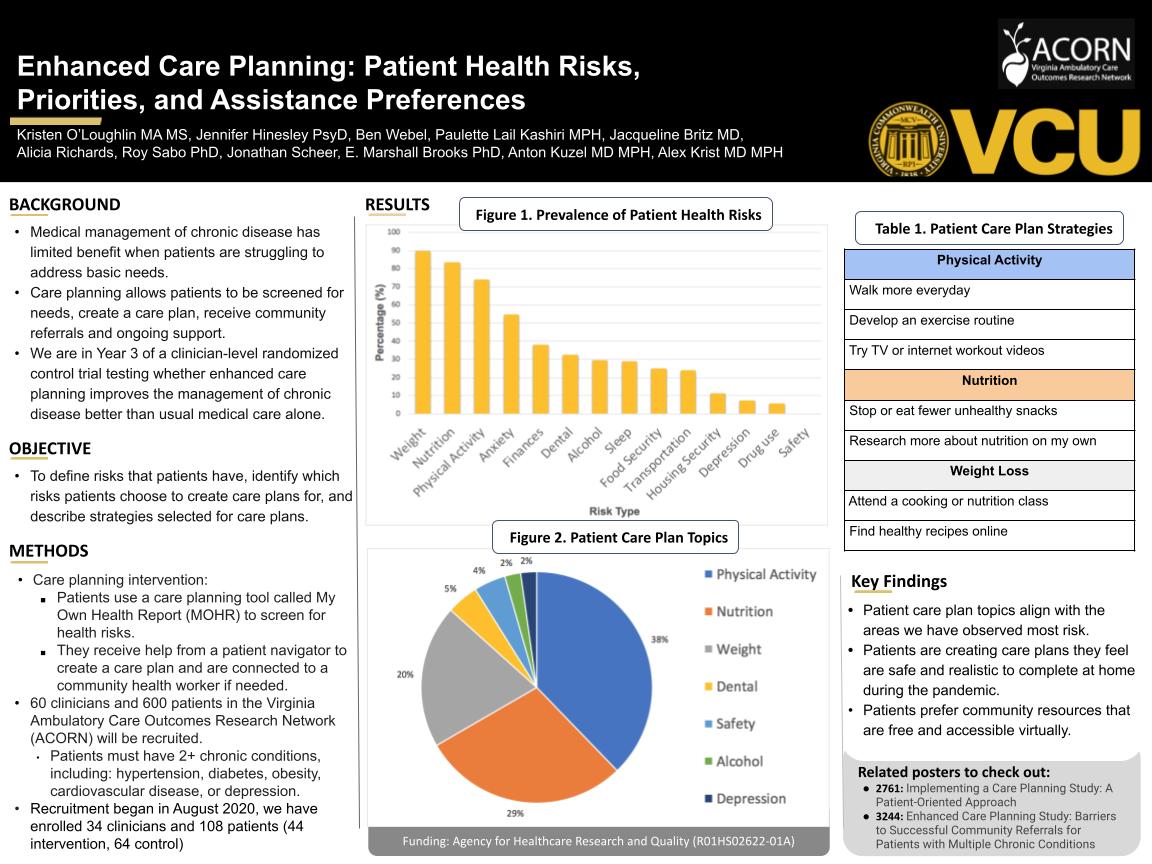
Context: Many patients with multiple chronic conditions (MCC) have unmet social needs, mental health challenges, and unhealthy behaviors that may compromise their health. Medical management of MCC may have limited benefit if patients are struggling to address basic needs. Care planning allows patients to be screened for needs, create a care plan, and receive support from a patient navigator and community health worker to help make desired changes. We are in the third year of a 5-year clinician-level randomized control trial testing whether enhanced care planning will help improve the management of chronic conditions better than traditional medical care alone. Objective: To define risks that patients have, identify which risks patients choose to create care plans for, and describe strategies selected for care plans. Methods: Sixty clinicians and 600 patients in the Virginia Ambulatory Care Outcomes Research Network (ACORN) will be recruited. Patients must have two or more chronic conditions, including cardiovascular disease, diabetes, obesity, or depression. From these 600 patients, 300 will be randomized to the care planning intervention and 300 to control (usual care). Patients in the intervention group will use an enhanced care planning tool called My Own Health Report (MOHR) to screen for health behavior, mental health, and social needs. They will receive help from a patient navigator to create a care plan and are connected to a community health worker if needed. Recruitment began in August 2020 and the first two waves of clinicians, 22 total, have been enrolled. Data sources for these analyses include the health risk assessment and care plans from MOHR. Expected Outcomes: Preliminary data shows that patients prioritize health behaviors such as nutrition, weight loss, and physical activity over mental health and social needs. Patients prefer strategies and community resources that are free and can be accessed from home, such as virtual nutrition counseling and exercise classes. Formal quantitative analyses will be presented. Conclusion: These findings help improve understanding of the mental health, health behavior, and social needs of patients with MCC. They also provide insight into how patients prioritize multiple needs and prefer to address them, which may inform future interventions and clinical care.
Jack Westfall
jwestfall@aafp.org 11/21/2021Terrific project. Great poster and abstract. Thanks for sharing at NAPCRG