PRP024: Detect and Save: Predicting and Preventing Clinical Deterioration Using Artificial Intelligence
Margaret Smith, MBA; Steven Lin, MD; Jerri Westphal, MSN, RN; Lisa Shieh; Ron Li, MD
Abstract
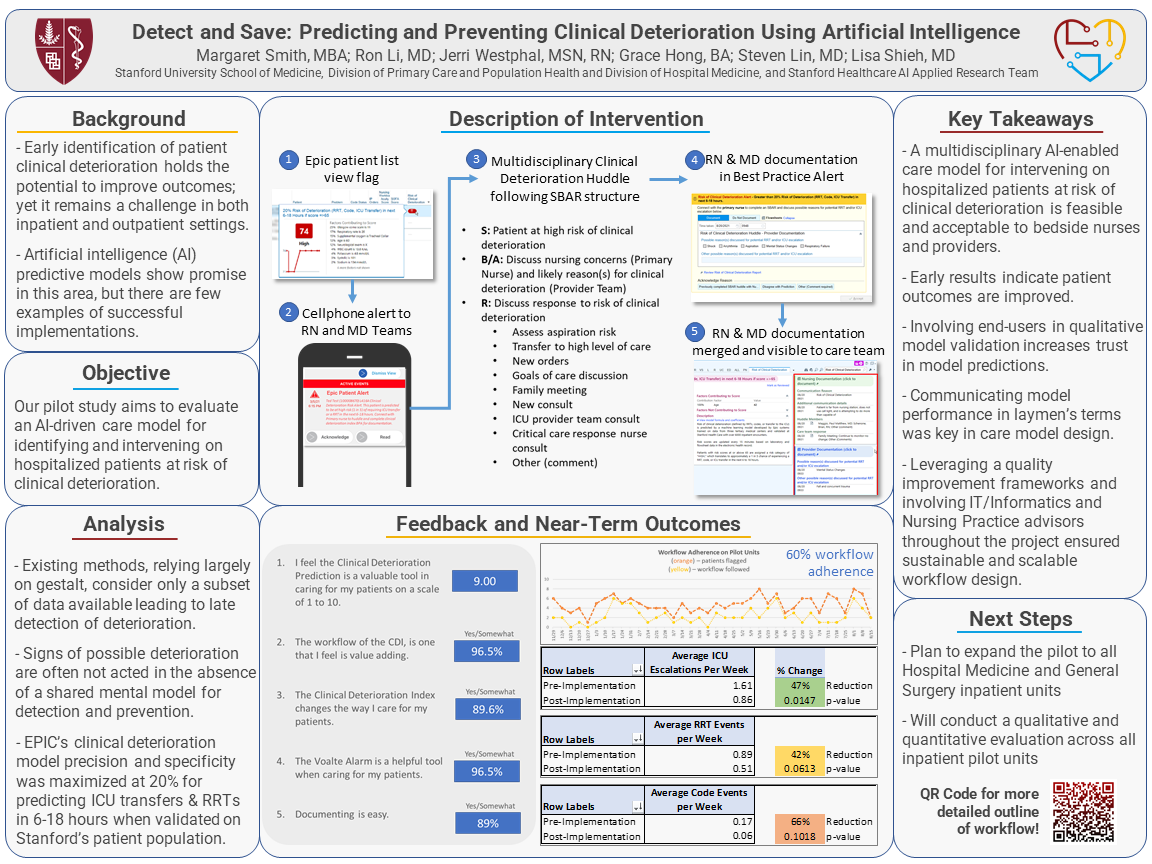
Context: Early identification of patient clinical deterioration holds the potential to decrease mortality and improve outcomes; yet it remains a challenge in both hospital and ambulatory settings. Artificial intelligence (AI) predictive models show promise in this area, but there are few examples of successful implementations in real-world settings. Objective: To evaluate the effectiveness of a clinically integrated AI-driven workflow for identifying and intervening on hospitalized patients at risk of clinical deterioration. Study design: Prospective cohort study using mixed methods to assess processes and outcomes with randomized delivery of model alerts. Setting: Inpatient adjustable acuity units in a large quaternary academic hospital. Quantitative data on processes and outcomes will be collected from the EHR. Interviews and surveys will be conducted with members of the multidisciplinary team. Population studied: All patients admitted to six medicine units, regardless of admission diagnoses. Intervention: An AI-driven work system comprised of 3 parts: an AI model that predicts clinical deterioration, an EHR best practice alert with or without a phone alert delivering model predictions to the clinical teams, and a multidisciplinary workflow called the “clinical deterioration huddle”. The AI model was created by Epic, prospectively validated on 6232 hospital encounters, and predicts ICU transfer, RRT or code events within 6 to 18 hours – estimated as an appropriate time interval by clinical stakeholders. Outcome measures: Primary outcomes: (1) code events per month; (2) ICU escalations per month; (3) rapid response team (RRT) activations per month; (4) patient mortality events per month. Secondary outcomes: (1) actions taken by the clinical team in response to model alert, based on documentation of clinical deterioration huddles in the EHR; (2) time between alert and completion of workflow; (3) clinical team members’ perceptions of workflow effectiveness. Results and outcomes to be reported: Our preliminary results piloting the AI enabled intervention on one unit over 17 weeks yielded promising findings. During the pilot, 77 patients were flagged by the model, and the multidisciplinary workflow was completed on 55% of flagged patients. Team members rated the intervention 8.33 out of 10 in terms of perceived value in patient care. We plan to expand the pilot and study for 6 months before reporting the final results of our primary and secondary outcomes.
Jack Westfall
jwestfall@aafp.org 11/21/2021Very interesting research. Great work. Thanks