PRP042: High Systolic Blood Pressure Reduction and Health Insurance Status in Community Health Centers
Annie Larson, PhD, MPH; Beverly Green, MD, PhD; Steele Valenzuela, MSc; Heather Angier, PhD, MPH; Miguel Marino, PhD; Treasure Allen, MPH; Nathalie Huguet, PhD
Abstract
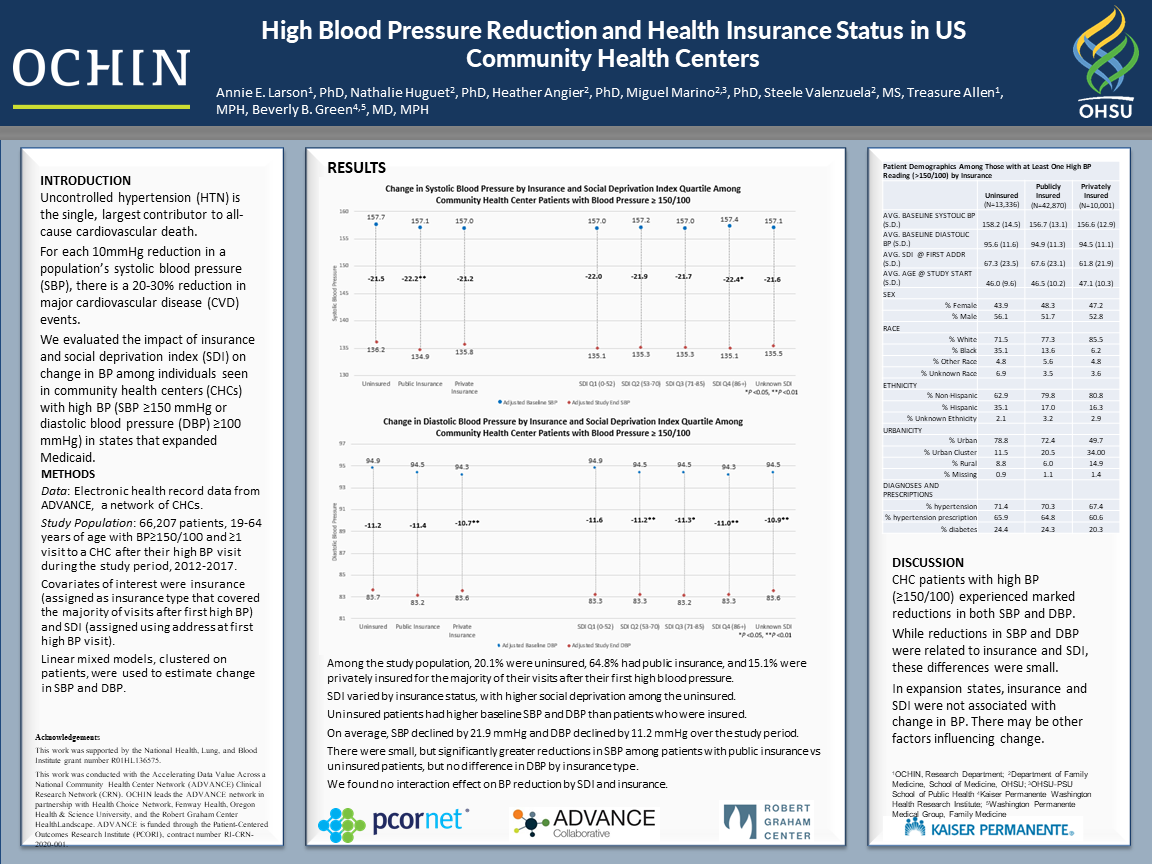
Context: Hypertension is a leading cause of cardiovascular disease (CVD) and death. For every 10mmHg decrease in systolic blood pressure (SBP) there is a 20-30% reduction in major CVD events and death. Individuals with very high BP, defined as SBP ≥150 mmHg or diastolic BP ≥100 mmHg, have greater CVD risk than those with BP that is not as high. Lack of health insurance is a risk factor for uncontrolled hypertension, but it is unknown whether having health insurance leads to greater reductions in BP. Objective: To estimate the relationship between health insurance type and patient’s community-level social deprivation index (SDI) on reduction of SBP. Study Design: Retrospective cohort study of electronic health record data from OCHIN, a network of community health centers that provide care to underserved populations. Population studied: Patients aged 19 and 64 (excluding pregnant women) with ≥1 very high BP reading and ≥1 follow-up visit between 01/01/2012-12/31/2017 (N=66,208). Outcome: Change in SBP over time using multilevel modeling to estimate the effect of health insurance and SDI while adjusting for other patient characteristics. Results: Patients had, on average,10 follow-up visits after the initial high BP with an average annual reduction in SBP of 3.2 mmHg over the study period. 66,208 (21.2% of the entire population) had a BP ≥150/100 mg and ≥1 follow-up visit with a BP; 70.6% had a hypertension diagnosis and 65.1% were prescribed hypertension medications. The majority had public insurance (mainly Medicaid) 64.8%, 20.1% were uninsured, and 15.1% had private insurance. In the covariate-adjusted model, compared to uninsured, public and private insurance were associated with significantly lower SBP (-3.7 mmHg, CI-3.0,-4.3 and -1.9 mmHg, -1.2,-2.6 respectively). When stratifying by insurance, we did not find differing effects by SDI, but did find differences by ethnicity. Conclusions: Having health insurance was associated with greater reductions in SBP than not having insurance. If confirmed in full analyses, providing insurance to all individuals could lead to significant reductions in CVD events and death.
Jack Westfall
jwestfall@aafp.org 11/21/2021Thanks for your terrific work on this research. Hope you can connect with us at the Robert Graham Center https://www.graham-center.org/rgc/home.html