PRP011: Association between physician continuity of care and patient outcomes: Evidence from Virginia all-payer claims database
Mingliang Dai, PhD; Lars Peterson, MD, PhD; Jill Shuemaker, RN, CPHIMS; Beth Bortz, MPP; Zachary Morgan, MS
Abstract
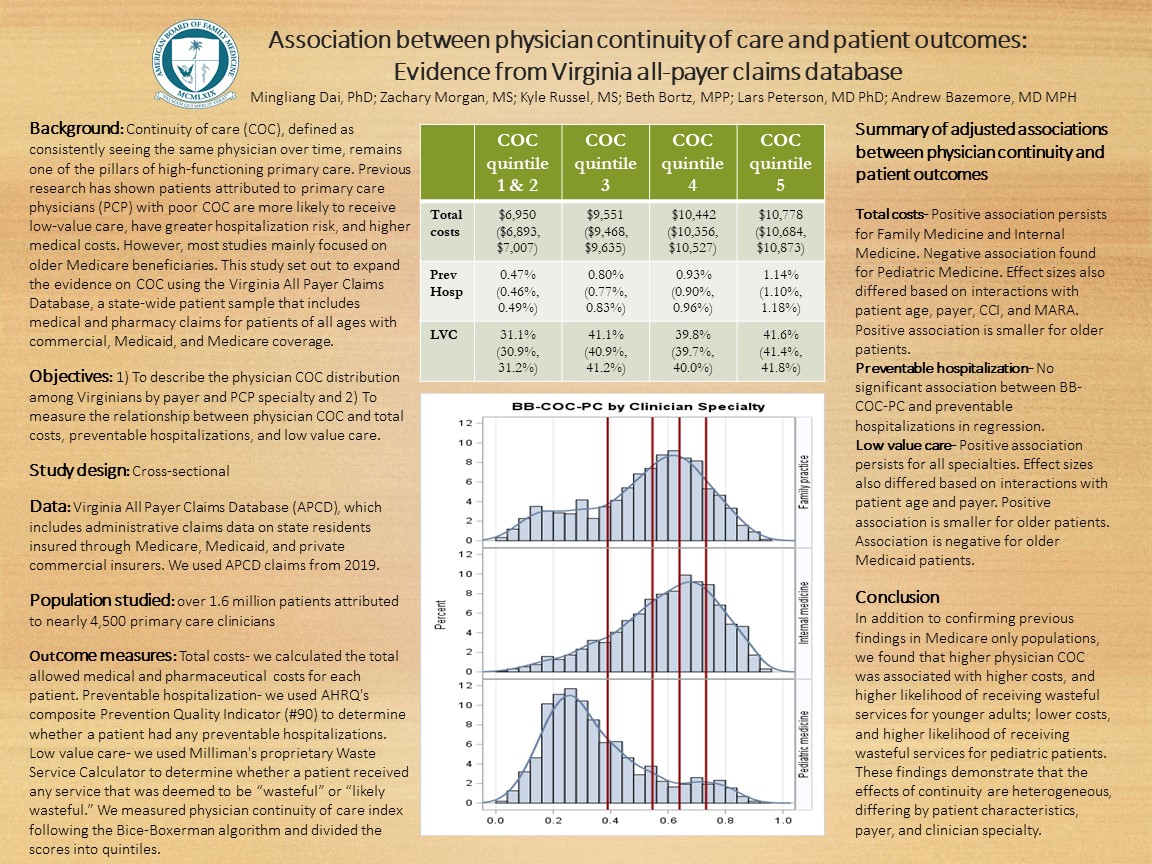
Context: Continuity of care (COC), defined as seeing the same physician over time, remains one of the pillars of a high-functioning primary care. Patients with poor COC with primary care physicians (PCP) are more likely to receive low-value care, have greater hospitalization risk, and higher medical costs. However, most studies mainly focused on older Medicare beneficiaries. This study set out to expand the evidence on COC in a state-wide patient sample that includes patients both young and old and with different insurance coverage.
Objectives: 1) To describe the COC distribution among Virginians by payer and PCP specialty. 2) To measure the relationship between COC and preventable hospitalization, total costs, and low value care.
Study design: Cross-sectional
Dataset: Virginia All Payer Claims Database (VA-APCD), which includes administrative claims data on state residents insured through fee-for-service Medicare, Medicare Advantage, Medicaid, and private commercial insurers. We used APCD claims from 2015.
Population studied: Over 1.3 million patients who received most of their care from 6329 PCPs including 2781 family physicians, 2235 internists, and 1313 pediatricians.
Outcome measures: We used AHRQ's composite Prevention Quality Indicator (#90) to measure whether a patient had any preventable hospitalization in 2015. For total costs, we summed outpatient, facility as well as prescription costs for each patient. For low value care, we used Milliman's proprietary Waste Service Calculator to calculate the proportion of services provided by PCP that was determined as wasteful relative to quality services. We measured continuity of care following the Bice-Boxerman method.
Analysis: We will plot the distribution of COC by patient's primary payer and attributed PCP's specialty. We will model the odds of having any preventable hospitalization in logistic regression models. We will model total costs using GLM with log link and normal distribution. We will model low value care using GLM. All models will adjust for patient and physician characteristics and account for repeated measure within same physician by including a physician random effect.
Results and conclusion: The analysis is still underway and will be ready for presentation by the time of the conference.
Objectives: 1) To describe the COC distribution among Virginians by payer and PCP specialty. 2) To measure the relationship between COC and preventable hospitalization, total costs, and low value care.
Study design: Cross-sectional
Dataset: Virginia All Payer Claims Database (VA-APCD), which includes administrative claims data on state residents insured through fee-for-service Medicare, Medicare Advantage, Medicaid, and private commercial insurers. We used APCD claims from 2015.
Population studied: Over 1.3 million patients who received most of their care from 6329 PCPs including 2781 family physicians, 2235 internists, and 1313 pediatricians.
Outcome measures: We used AHRQ's composite Prevention Quality Indicator (#90) to measure whether a patient had any preventable hospitalization in 2015. For total costs, we summed outpatient, facility as well as prescription costs for each patient. For low value care, we used Milliman's proprietary Waste Service Calculator to calculate the proportion of services provided by PCP that was determined as wasteful relative to quality services. We measured continuity of care following the Bice-Boxerman method.
Analysis: We will plot the distribution of COC by patient's primary payer and attributed PCP's specialty. We will model the odds of having any preventable hospitalization in logistic regression models. We will model total costs using GLM with log link and normal distribution. We will model low value care using GLM. All models will adjust for patient and physician characteristics and account for repeated measure within same physician by including a physician random effect.
Results and conclusion: The analysis is still underway and will be ready for presentation by the time of the conference.
Jack Westfall
jwestfall@aafp.org 11/21/2021Terrific project. Great poster and abstract. Thanks for sharing at NAPCRG