PRP100: Using Electronic Health Records to Study Nativity as a Cardiovascular Disease Risk Factor in Community Health Center Patients
Jennifer Lucas, PhD; Miguel Marino, PhD; Elena Byhoff, MD; Sophia Giebultowicz, MA; Danielle Crookes, DrPH; Kristin Scott, MPH; John Heintzman, MD, MPH; Jorge Kaufmann, MS; David Boston, MD, MS; David Ezekiel-Herrera, MS
Abstract
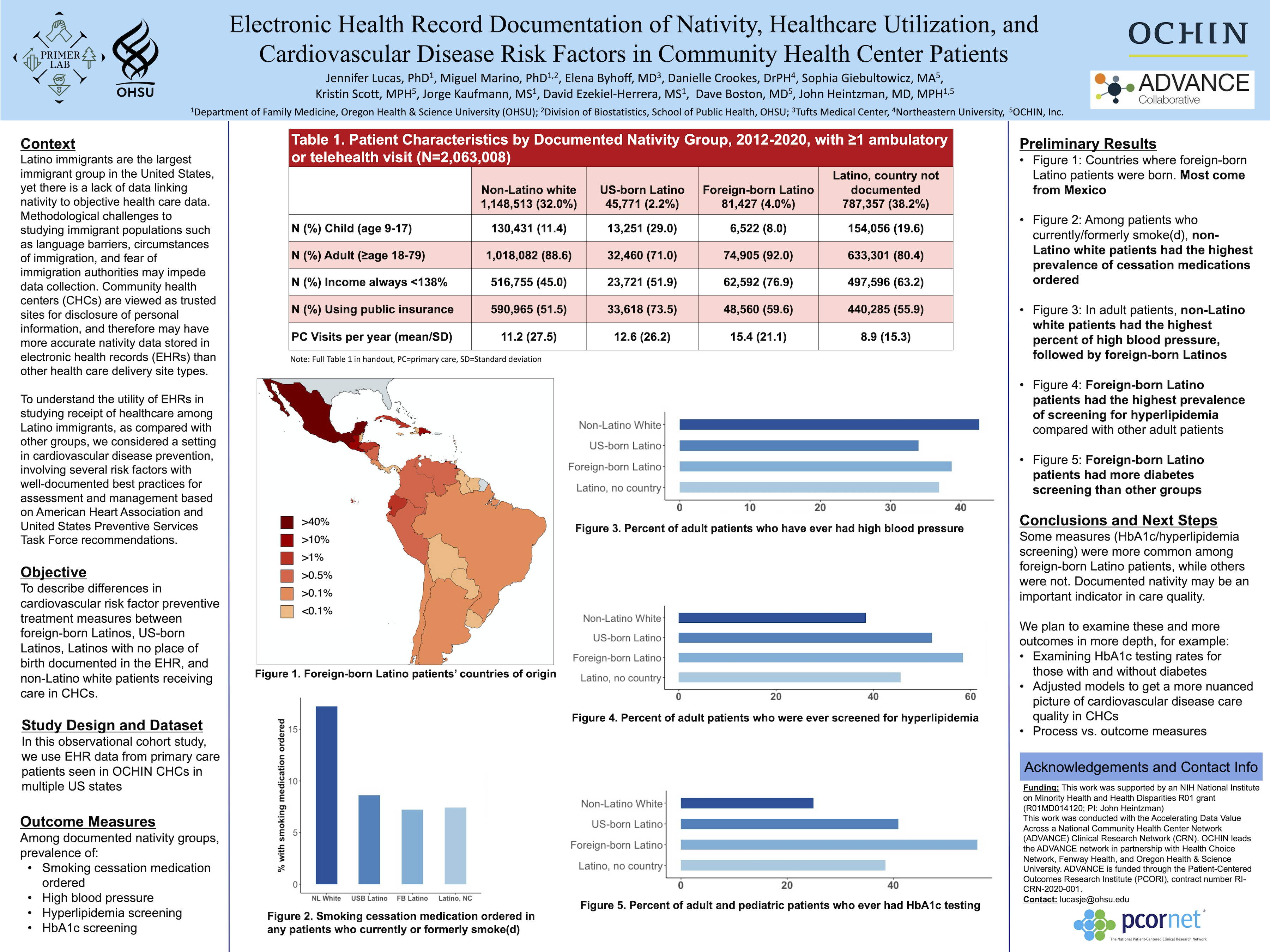
Objective: To describe differences in utilization and rates of cardiovascular risk factors between foreign-born Latinos, US-born Latinos, and non-Hispanic white patients who receive care in CHCs.
Study Design: Observational cohort study
Dataset: Electronic health record data from primary care patients seen in OCHIN CHCs in multiple US states.
Population studied: Our data contain 1,482,314 patients aged 9-79 years with ≥1 ambulatory/telehealth visit in an OCHIN clinic from 1/1/2012-12/31/2020. Of these,155,663 (10.5%) have nativity data reported in the EHR.
Outcome measures: Screening/monitoring rates of blood pressure, hyperlipidemia, HbA1c, smoking cessation service, and aspirin use per American Heart Association and United States Preventive Services Task Force recommendations, along with documentation of nativity
Results: We anticipate that foreign-born Latinos will be less likely to receive recommended cardiovascular preventive services than US-born Latinos and non-Hispanic white CHC patients.
Conclusions: Current and accurate data are necessary to identify and address health disparities. This study will help primary care clinicians and researchers identify populations who may be at risk for disparate preventive care measures.
Diane Harper
harperdi@med.umich.edu 11/21/2021Interesting racial comparisons. US born Latinos have significantly higher use of public insurance - is that a process of the FQHC that automatically helps them enroll for payment?