PRP027: Documenting and extracting patient-level social risk data in electronic health records: a systematic review
Shyam Patel; Gaia Linfield; Hee Joo Ko; Emilia De Marchis, MD, MAS; Laura Gottlieb, MD, MPH; Matthew Pantell, MD, MS; Nina Singh
Abstract
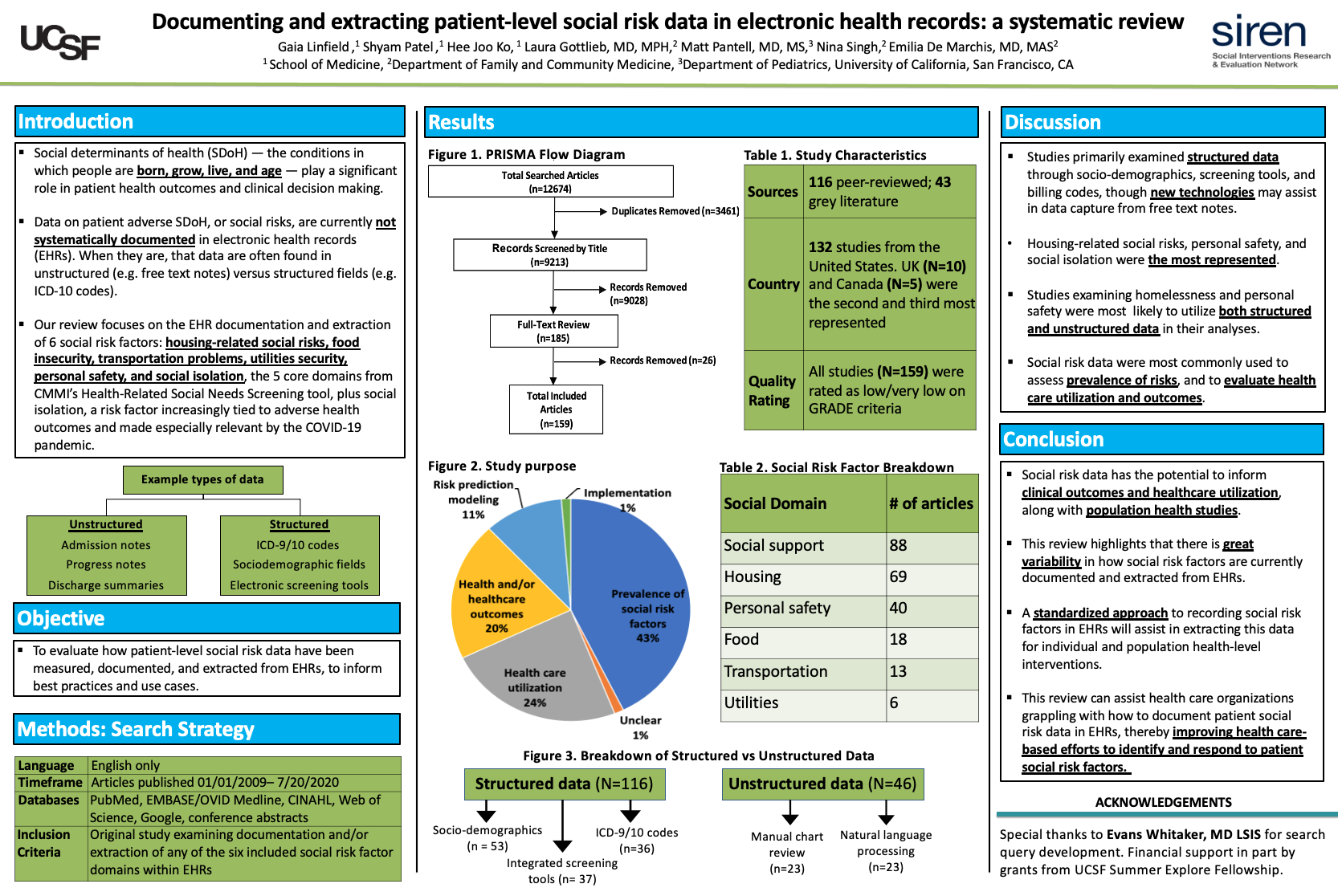
Context: There are growing efforts and incentives to screen patients for adverse social determinants of health, or social risk factors, within health care settings, but no standardized documentation guidelines exist. Patient social risk data are currently inconsistently documented in electronic health records (EHRs), making it challenging to extract information for individual or population health management efforts. Objective: To evaluate how patient-level social risk data have been measured, documented, and extracted from EHRs to inform best practices and use cases. Study Design & Dataset: Systematic review within Pubmed, EMBASE, CINAHL, Web of Science, Google, clinicaltrials.gov, and conference abstracts. Study quality was assessed by the Grading Recommendations Assessment Development and Evaluation (GRADE) criteria. Population Studied: Articles published in peer-reviewed or grey literature from 1/1/2009 to 7/20/20 that included EHR documentation and extraction of at least one of the following social risk factors: housing, transportation, food security, utilities, personal safety, and social isolation. Outcome measures: Data extraction included: study population, setting, metrics to define social risk domains, method of social risk factor documentation (e.g. billing codes vs. free text), social risk data extraction technique, and study outcomes. Results: Our search yielded 9,213 unique articles. After initial title and abstract screen, 147 articles underwent full-text review and 134 articles met study inclusion criteria. Based on sample size and study design, 99% (N=133) were rated as low or very low quality. Housing stability (66/134, 49%), personal safety (40/134, 30%), and marital status (37/134, 28%) were the most commonly included social risk domains. Across domains, social risk factors were primarily documented in structured EHR fields, including under socio-demographics, integrated screening tools, and billing codes. 16% (N=21) of studies examined social risk documentation in unstructured fields, such as free-text clinical notes. Conclusions: Upon completion of the qualitative review, we will highlight patterns of EHR-based social risk data documentation and extraction. Assessing current methods and use cases will inform future standardization efforts. Examining lessons learned will assist health care organizations in their efforts to identify and respond to patient social risk factors.
Jack Westfall
jwestfall@aafp.org 11/21/2021So great to see students presenting at NAPCRG. Hope to see you next year at NAPCRG 2022!. Very interesting research. Great work. Thanks