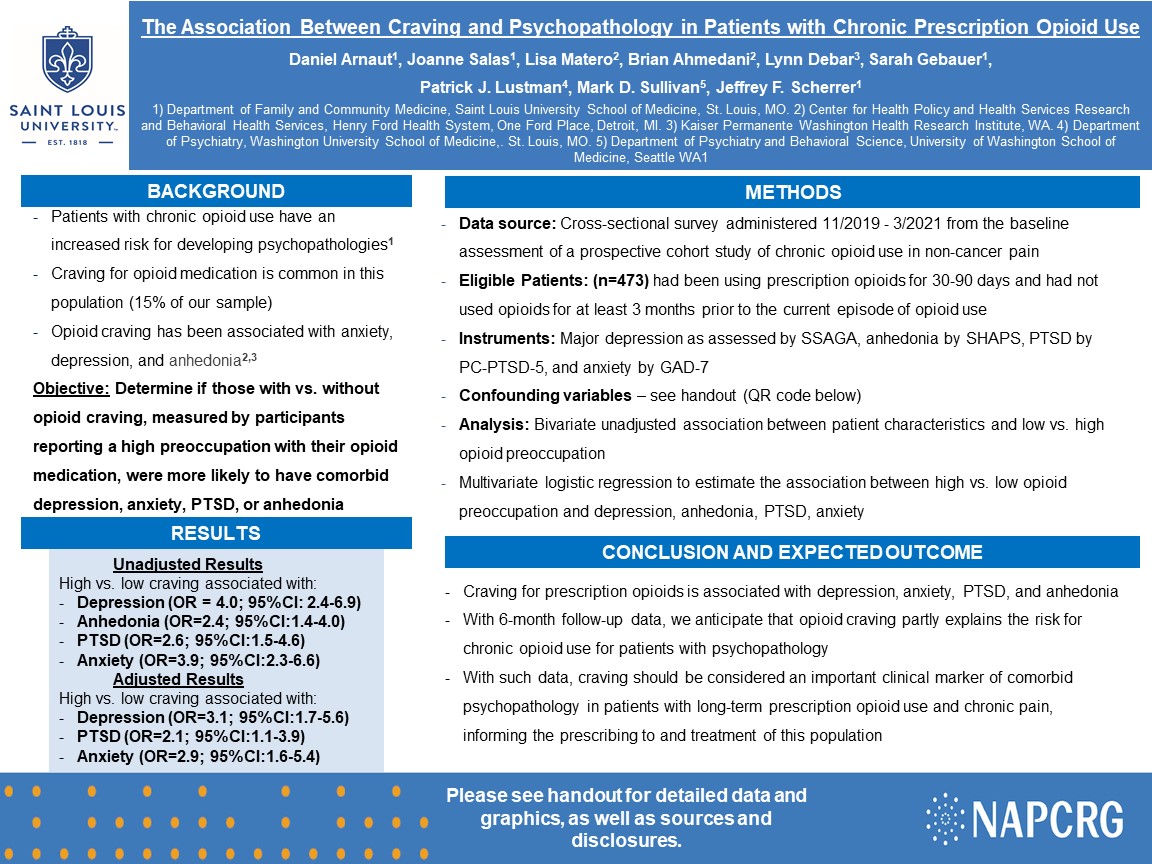
PRP085: The association between craving and psychopathology among patients with chronic prescription opioid use.
Daniel Arnaut, BS; Patrick Lustman, PhD; Joanne Salas, MPH; Jeffrey Scherrer, PhD; Lisa Miller-Matero, PhD
Abstract
Context: Patients with psychopathology are more likely to become long-term prescription opioid users and develop opioid dependence. Long-term opioid users often experience craving, described as a strong desire to use opioids and/or obsessive thoughts about opioids. Opioid craving has been shown to be more common among patients with non-cancer pain, depression and anxiety. Craving may be a factor common to chronic opioid use and psychopathology. Objective: Determine if those with vs. without opioid craving, measured by participants reporting a high preoccupation with their opioid medication, were more likely to have comorbid depression, anxiety, PTSD, or anhedonia. Study design: Cross-sectional Data set: Survey data obtained from the baseline assessment of a prospective cohort study of chronic opioid use in non-cancer pain. Population studied: The first 473 subjects who completed the baseline assessment between 11/2019 to 3/2021 were included if they had been using prescription opioids for 30-90 days and had not used opioids for at least 3 months prior to the current episode of opioid use. Outcome measures and instruments: major depression as assessed by SSAGA, anhedonia by SHAPS, PTSD by PC-PTSD-5, and anxiety by GAD-7. Analysis: Multivariate logistic regression. Results: Patients were on average 52.2 (SD±12.5) years of age, 68% female and 67% white race. Overall, 15% reported opioid craving. Results of unadjusted analysis revealed that, compared to those without opioid craving, those with craving were significantly more likely to have depression (OR=4.03; 95%CI:2.35-6.93), anhedonia (OR=2.36; 95%CI:1.40-3.97), PTSD (OR=2.61; 95%CI:1.48-4.60) and anxiety (OR=3.89; 95%CI:2.28-6.64). After adjusting for age, gender, race, daily vs non-daily opioid use, high pain severity, high pain interference, alcohol misuse and any illegal drug use, those with vs. without opioid craving were more likely to have major depression (OR=3.06; 95%CI:1.68-5.56), PTSD (OR=2.08; 95%CI:1.11-3.88), and anxiety (OR=2.93; 95%CI:1.59-5.37). Expected outcomes: After including 6-month follow-up data, we anticipate finding that opioid craving partly explains the risk for chronic opioid use for patients with psychopathology. If the anticipated findings are confirmed, craving should be considered an important clinical marker of comorbid psychopathology in patients with long-term prescription opioid use and chronic pain, informing the prescribing to and treatment of this population.
Diane Harper
harperdi@med.umich.edu 11/21/2021thank you for sharing your work with NAPCRG.