PCR019: Comparing race and ethnicity across safety-net and non-safety net practices pre- and post-an HIV screening alert
Thomas Ludden, PhD; Jeremy Thomas, MSW; Lindsay Shade, MHS, PA-C; Hazel Tapp, PhD, PhD; Michael Leonard
Abstract
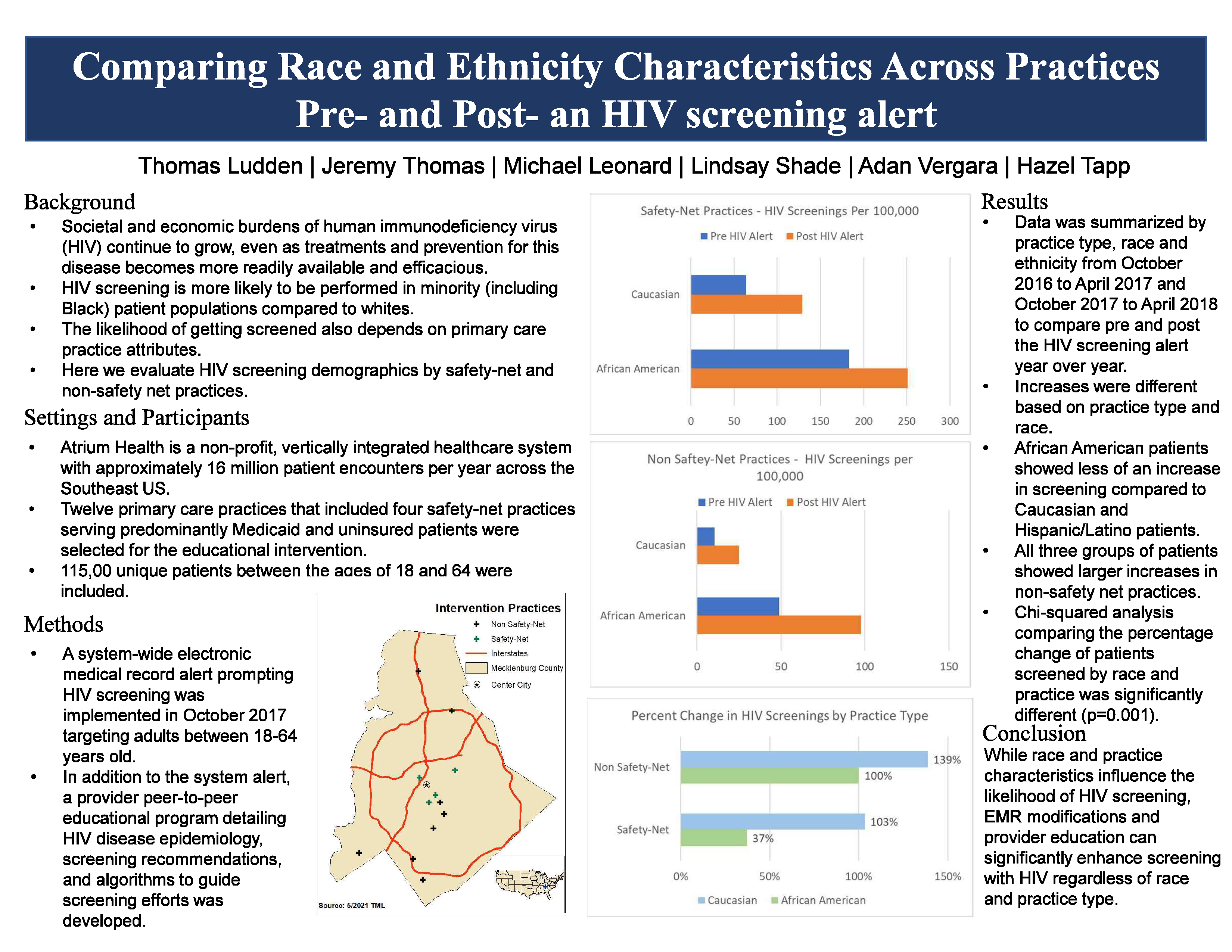
CONTEXT: Societal and economic burdens of human immunodeficiency virus (HIV) continue to grow, even as treatments and prevention for this disease becomes more readily available and efficacious. HIV screening is more likely to be performed in minority (including Black) patient populations compared to whites. The likelihood of getting screened also depends on primary care practice attributes. OBJECTIVE: Evaluate HIV screening demographics by safety-net and non-safety net practices. STUDY DESIGN and ANALYSIS: Pre-post analysis. SETTING: Atrium Health is a non-profit, vertically integrated healthcare system with approximately 16 million patient encounters per year across the Southeast US. POPULATION STUDIED: Twelve primary care practices, including four safety-net practices serving predominantly Medicaid and uninsured patients, with over 115,00 patients between the ages of 18 and 64 were selected for the educational intervention. INTERVENTION/INSTRUMENT: A system-wide electronic medical record alert prompting HIV screening was implemented in October 2017 targeting adults between 18-64 years old. In addition to the system alert, a provider peer-to-peer educational program detailing HIV disease epidemiology, screening recommendations, and algorithms to guide screening efforts was developed. OUTCOME MEASURES: HIV screenings. RESULTS: From October 2016– April 2017, 3,413 patients were screened for HIV at the twelve participating primary care practices. Immediately after the HIV alert activation, from October 2017 – April 2018, 6,256 patients were screened, resulting in an 83% increase in screening. However, increases were different based on practice type, race and ethnicity. Black patients in safety net clinics had higher screening rates prior to the alert and showed less of an increase in screening (37%) compared to whites (102%) after the alert was activated. Hispanic/Latino patients showed similar increases at both safety net (99%) and non-safety net (108%) practices. Both Black and white patients showed larger increases of 99% and 139% in non-safety net clinics. Chi-squared analysis comparing the percentage of patients screened during these time periods was significantly different (p=0.001). CONCLUSION: While race and practice characteristics influence the likelihood of HIV screening, EMR modifications and provider education can significantly enhance screening and care for patients with HIV regardless of race and practice type.
Jack Westfall
jwestfall@aafp.org 11/19/2021Great poster and abstract. Thanks