PCR039: Models of Care for Pregnant Women with Opioid Use Disorder: A Multisite Pilot Study (Pearls)
Sherry Weitzen, MD, PhD; Kristin Ashford, PhD, NP, PhD, WHNP-BC; Kara McKinney, MA; Jessica Coker, MD; Marcela Smid, MD, MA, MS
Abstract
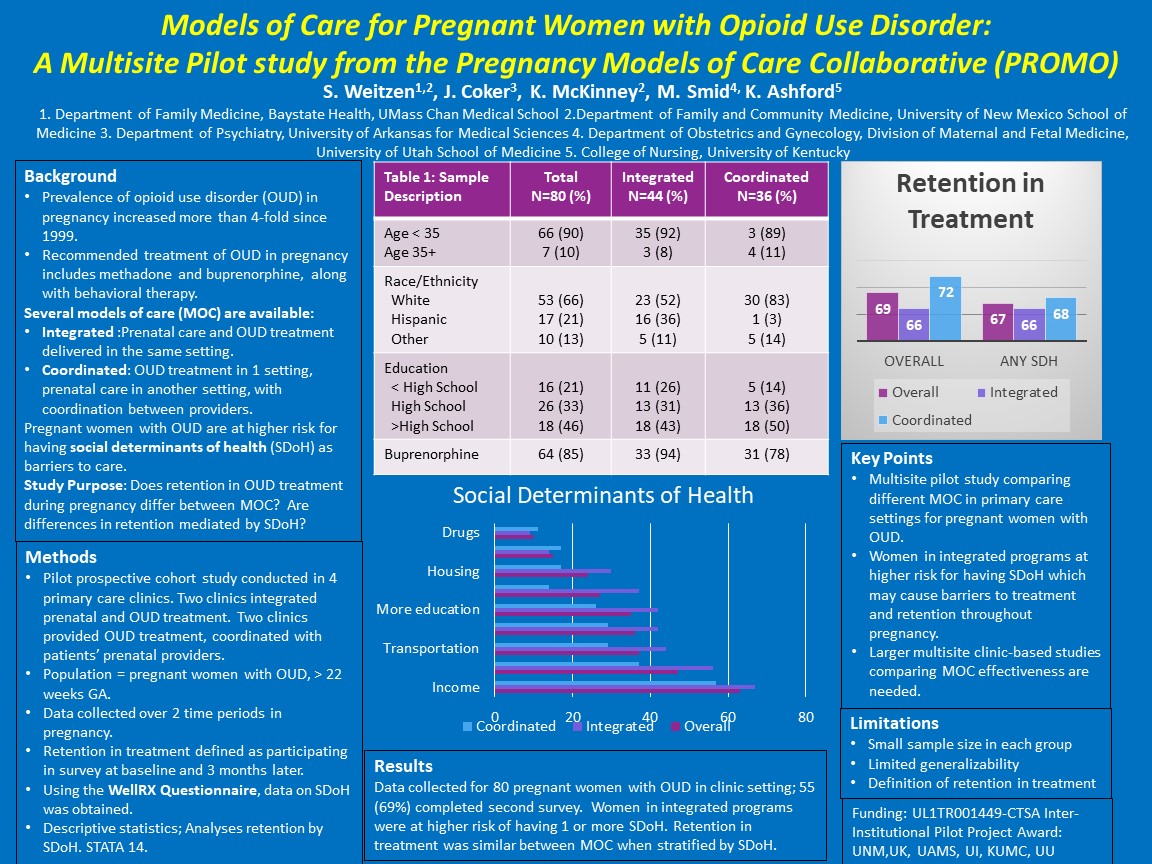
Context: Pregnancy is an opportunity to engage women with opioid use disorder (OUD) in treatment. Models of care (MOC) for pregnant women with OUD vary widely, resulting in challenges for research. Objective: To enhance research capacity, we formed a multi-site collaborative and conducted a pilot study between 4 treatment clinics (UAMS, UK, UNM, UU) with dissimilar MOCs. Presented here are preliminary findings and comparisons of retention in treatment across MOCs. Study Design and Analysis: We conducted a multisite prospective study among pregnant with OUD who were in treatment for OUD during pregnancy. Data were collected during pregnancy at 2 time points. Descriptive statistics were computed. Setting: All 4 sites provided outpatient treatment for OUD among pregnant women; 2 sites provided integrated OUD treatment and prenatal care (Integrated; UU, UNM); 2 sites provided treatment of OUD in coordination with patients’ obstetric providers (Coordinated; UAMS, UK). Population: Eligibility included: > 18 years; gestational age > 22 weeks, receiving medication for OUD, English speaking, consented. Intervention/Instrument: We developed and tested an intake questionnaire administered to participants while waiting for clinic appointments, including social determinants of health (SDH). We collected mental health, comorbidities and demographic data. Outcome Measures: We compared retention in treatment operationalized as completion of questionnaire at second time point between Integrated vs. Coordinated treatment for OUD with prenatal care. We considered SDH as a possible confounder. Results: We reached our recruitment goal of 80 women with OUD who completed the initial questionnaire (UAMS=16, UK=20, UNM=20, UU=24). Mean age was 29; 66% were White, non-Hispanic; 79% graduated from high school; 24% were married; and 78% reported the father of the baby was involved in this pregnancy. Overall, demographic characteristics across sites were similar. Women in integrated treatment had higher proportions of any SDH compared to coordinated treatment (88% vs. 80%). Retention in study was lower for Integrated compared to Coordinated treatment (66% vs 72%), but similar when stratified by having any SDH. Conclusion: This small multisite pilot study provides a foundation of future research to study pregnant women with opioid use disorder. Comparisons between integrated versus coordinated care suggest similar retention rates when stratified by social determinants of health.
Jack Westfall
jwestfall@aafp.org 11/20/2021Thanks for your terrific work on this research. Hope we can connect.