PCR081: What do self-reported social risk and community-level social contextual factors tell us about diabetes self-management?
Sarah Alowdi; José Parra, BS; Danielle Hessler Jones, PhD
Abstract
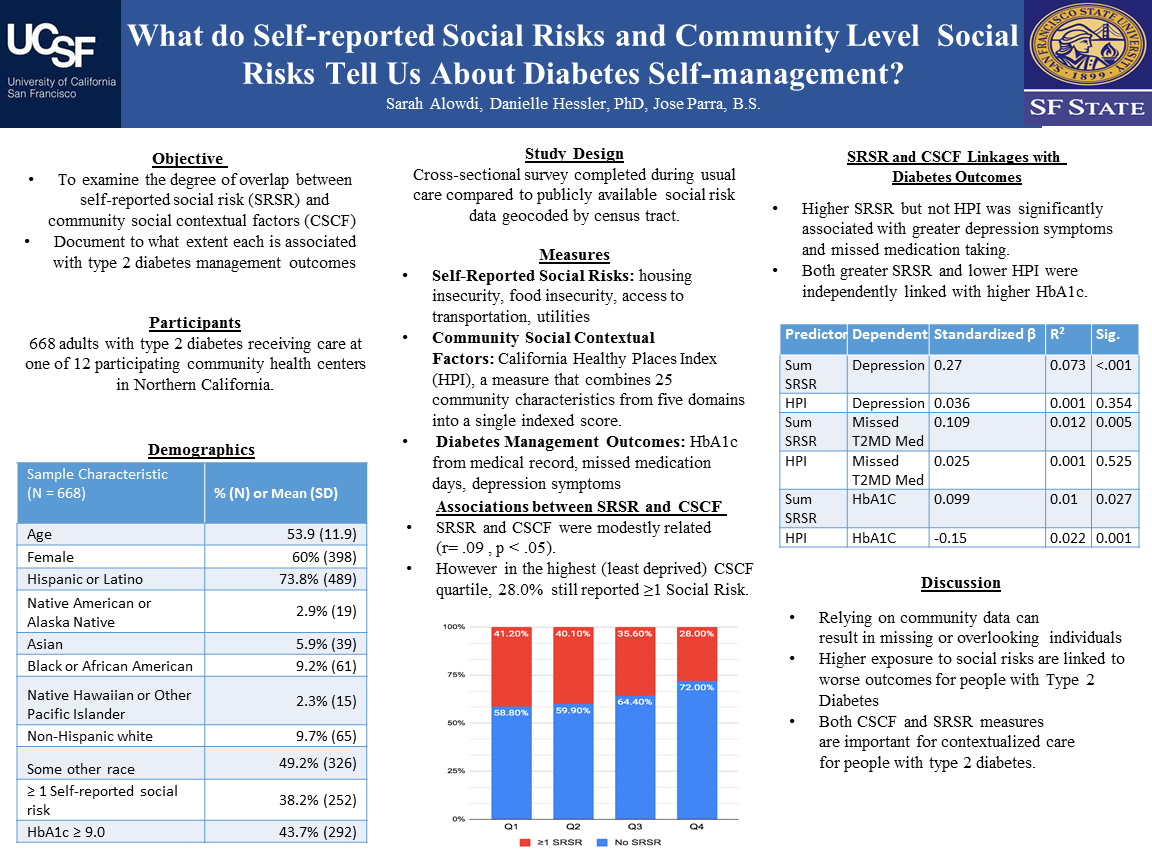
Context: Higher exposure to social risks, such as food and housing insecurity are linked to worse outcomes for people with type 2 diabetes (T2DM). Social risks can be assessed at the individual-level (self-report of personal experience) and in aggregate at the community level (e.g. census data). What is less understood is how self-reported vs. community level information compare to one another, and which is most relevant for understanding individuals’ T2DM management. Objective: To examine the degree of overlap between self-reported social risk (SRSR) and community social contextual factors (CSCF), and document to what extent each is associated with T2DM management. Study Design: Cross-sectional survey geocoded and linked to publicly available data on CSCF. Setting: 12 community health centers in the San Francisco Bay Area. Population: 668 adults with T2DM. Measures: SRSR was assessed through four binary (yes/no) items related to housing instability, food insecurity, access to transportation, and difficulties paying bills. CSCF was assessed by the California Healthy Places Index (HPI), a measure that combines 25 community characteristics from five domains (neighborhood and built environment, health/health care, social/community context, education, economic stability) into a single indexed percentile score (0-100%). T2DM management outcomes included HbA1c from medical records, self-reported missed medication days and depression symptoms (PHQ8). Results: 38.2% (n=252) of our sample endorsed ≥1 SRSR. HPI quartiles yielded the following distribution: Q1=31.7% (n=211); Q2=30.3% (n=202); Q3=24.0% (n=160); Q4=14.0% (n=93). 10.4% of individuals in Q4 endorsed ≥1 SRSR (vs. 34.7% in Q1). A sum of endorsed SRSR items were significantly, but modestly correlated with HPI (r =-0.09, p = 0.02). Individual SRSR items were similarly modestly associated with corresponding community-level contributors to HPI. SRSR but not HPI was significantly associated with individuals’ depression symptoms (b = .27, p <.001) and missed T2DM medications (b =.11, p = .005). Both greater SRSR (b =.10, p = .03) and lower HPI (b =-.15, p =.001) were independently linked with higher HbA1c. Conclusions: Findings align with previous work noting limited overlap between SRSR and CSCF data. Relying on CSCF data alone can result in missing or overlooking individuals experiencing social risks. This shows that both CSCF and SRSR measures are important for contextualized care with people with T2DM.
Jack Westfall
jwestfall@aafp.org 11/20/2021Thanks for your terrific work on this research. Hope we can connect.