PCR052: Planning, operationalizing, and evaluating patient partners’ engagement in primary care research: a logic model
Mathieu Bisson, MA; Maud-Christine Chouinard, PhD, RN; Frederick Kris Aubrey-Bassler, MD, MSc; Fred Burge, MD; Shelley Doucet, PhD, RN; Vivian Ramsden, PhD, BSN, MS, RN, MCFP (Hon.); Andre Gaudreau; Judy Porter; Mireille Lambert, MA; Dana Howse, PhD; Olivier Dumont-Samson, MA; Catherine Hudon, MD, PhD; Charlotte Schwarz, MA; Donna Rubenstein, BA, MBA; Cathy Scott; LINDA WILHELM; Marilyn Macdonald, PhD, RN; Alannah Delahunty-Pike, MSc
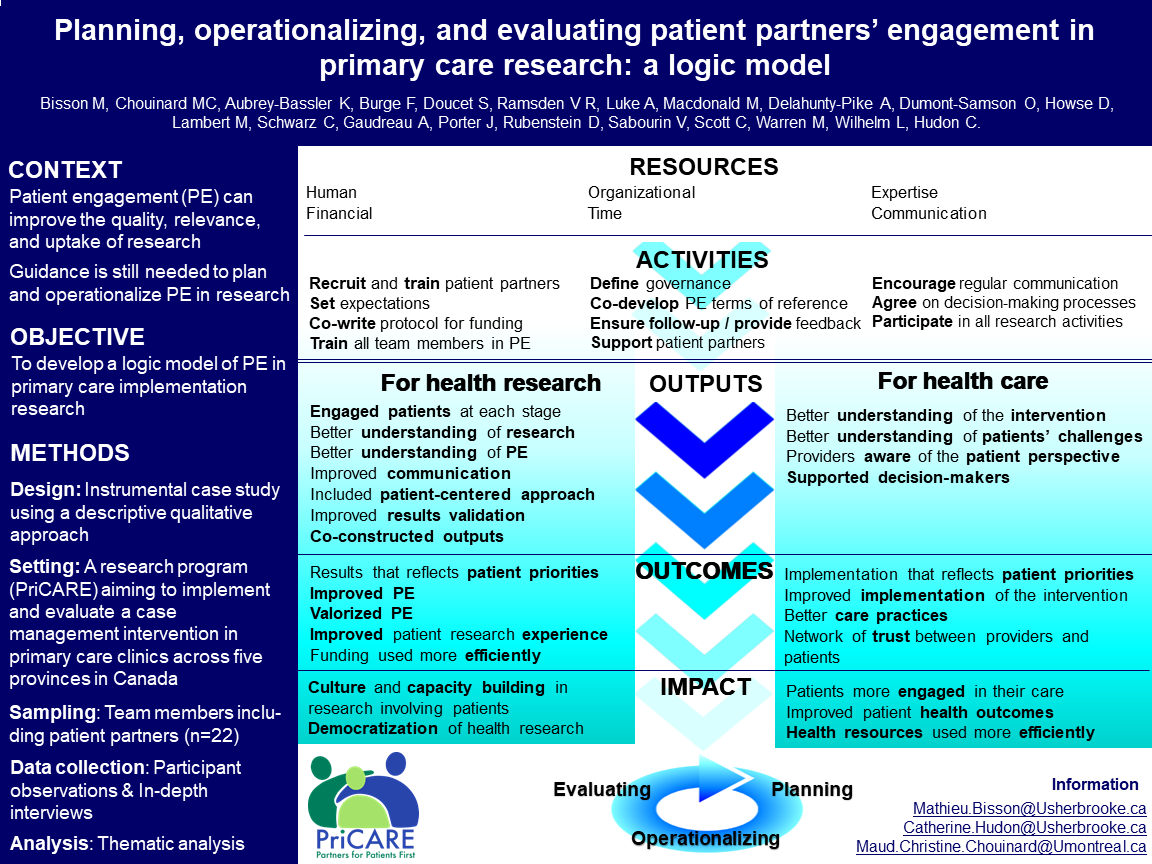
Context. There is growing evidence supporting patients’ engagement (PE) in primary care research to improve the quality, relevance, and uptake of research. However, guidance is still needed to plan and operationalize this engagement during the research process. Objective. To develop a logic model illustrating empirically the causal links between context, resources, activities, and expected outcomes of PE in an implementation research program in primary care. Study design. Instrumental case study. Setting. A research program (PriCARE) aiming to implement and evaluate a case management intervention (CMI) in primary care clinics across five provinces in Canada. Population studied. Research team members. Methods. Data collection. Participant observation and in-depth interviews (n=22) conducted by two independent research assistants with research team members: principal investigators (n=5); co-investigators (n=2); research coordinators and assistants (n=8); and patient partners (n=7). Analysis. Deductive thematic analysis using components of the logic model as coding categories. All data were coded using NVivo 12 software. Data were reduced and organized in a first logic model version. Team meetings helped to refine the logic model. The final version was validated by all research team members. Results. The logic model provides an empirical illustration of the relationship between context, resources, activities, and expected outcomes for PE. Mobilized resources (human, financial, organizational, and communicational) allow research team members to be involved in many activities related to PE: recruitment, training, and support of patient partners; development of a governance structure; participation in research activities; agreement on decision-making processes; training and support of clinicians; development of tools for patients’ involvement in the CMI. These activities lead to the following benefits for health research: improved communication amongst all team members, results and knowledge translation; development of a PE culture; capacity building; democratization of health research; and for healthcare: improved implementation of the intervention; improved patient engagement in their care; better health outcomes and resource utilization; support of decision-makers and clinicians; and better practices. Conclusions. The logic model may be useful for the planning, operationalization and evaluation of PPE in primary care research programs.
Jack Westfall
jwestfall@aafp.org 11/20/2021awesome work engaging community and patients. thanks for this work,