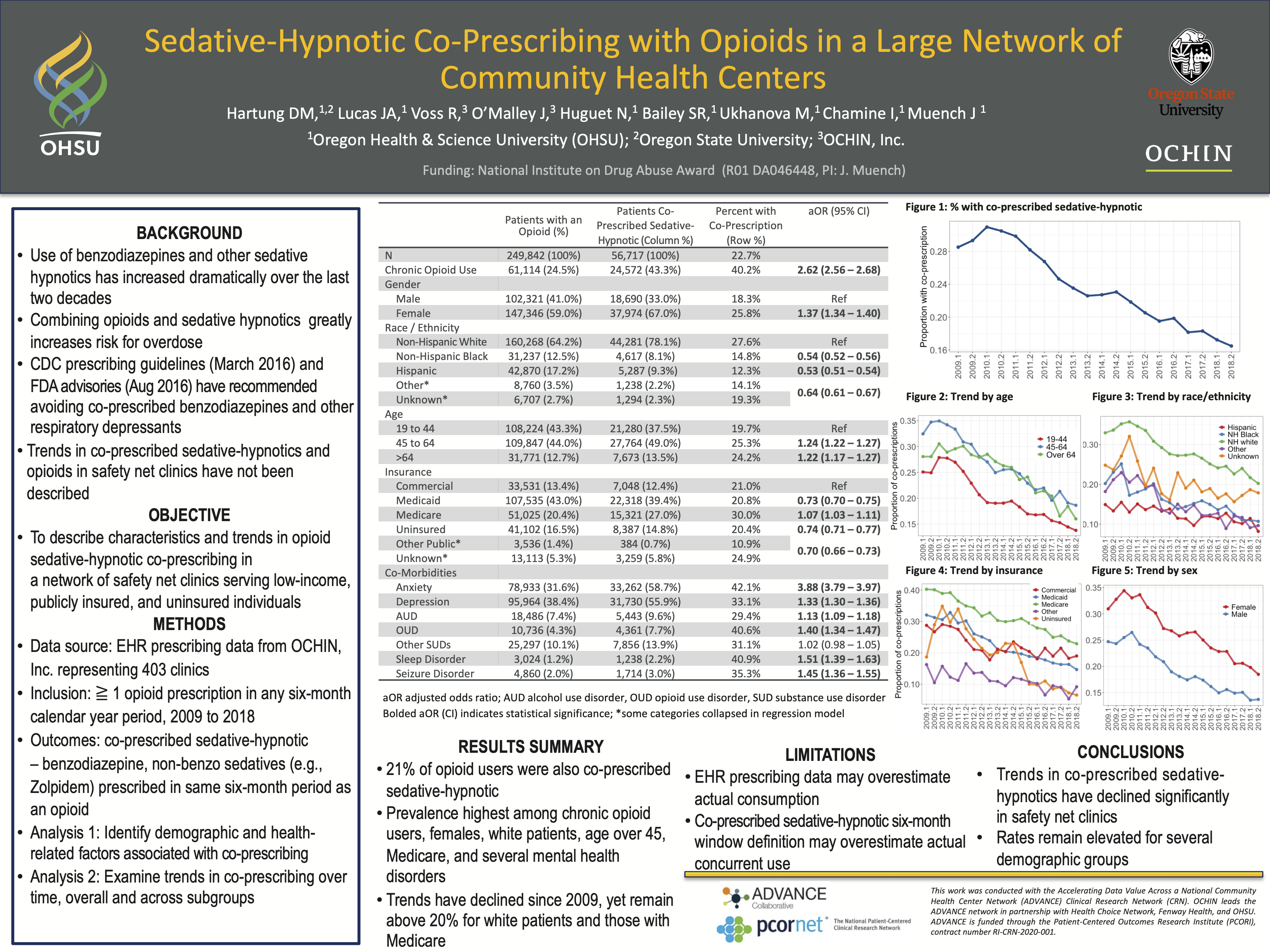
PCR063: Sedative-hypnotic Co-prescribing with Opioids in a Large Network of Community Health Centers
Daniel Hartung, MPH, PharmD; Jennifer Lucas, PhD; Robert Voss, MS; Jean O'Malley, MPH, PStat; Nathalie Huguet, PhD; Steffani Bailey, PhD; Maria Ukhanova, MD, PhD; Irina Chamine, PhD; John Muench, MD, MPH
Jack Westfall
jwestfall@aafp.org 11/20/2021very important topic. hope to see more come from this study. thanks.