PCR007: Analgesic Methadone Prescribing in Community Health Centers among Patients with Chronic Pain (Pearls)
Steffani Bailey, PhD; Robert Voss, MS; Irina Chamine, PhD; Daniel Hartung, MPH, PharmD; Nathalie Huguet, PhD; Gordon Barker, MS; Miguel Marino, PhD; Jean O'Malley, MPH, PStat; John Muench, MD, MPH
Abstract
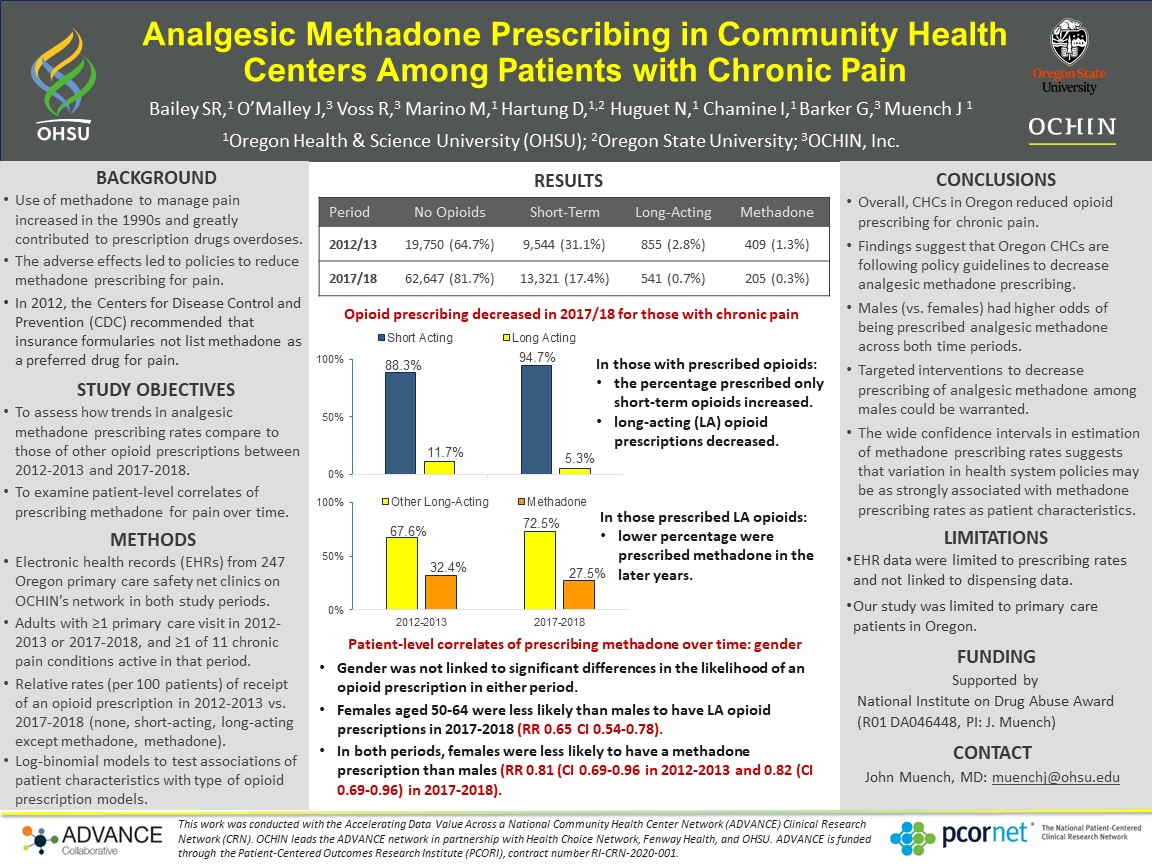
Context: Use of methadone to manage pain began increasing in the 1990s and became a significant contributor to overdoses caused by prescription drugs. These adverse outcomes led to advisories and policies related to methadone prescribing, including a 2012 CDC recommendation that insurance formularies not list methadone as a preferred drug for pain. Objectives: To examine patient-level correlates (age, gender, race/ethnicity) of prescribing methadone for chronic pain over time and how changes in analgesic methadone prescribing rates compare to those of other opioid prescriptions between 2012-2013 and 2017-2018. Study Design: Cross-sectional at two time points. Dataset: Electronic health records (EHR) from 247 Oregon primary care safety-net clinics on OCHIN’s EHR network in both study periods. Population studied: Adults (≥18 years of age) with ≥1 primary care visit to a study clinic in 2012-2013 or 2017-2018 and ≥1 of 11 chronic pain conditions (N=30,778 in 2012-2013; N=75,525 in 2017-2018) Outcome Measures: Patients with an opioid prescription (classified as none, short-acting, long-acting other than methadone, methadone) (rate/100 patients). Results: Prescription rates for all opioid types decreased markedly from 2012-2013 to 2017-2018; the percent of patients with no opioid prescription significantly increased. Relative prescription rates (RR) in 2017-2018 compared to 2012-2013 were lowest for methadone (RR=0.20, 95%CI 0.17-0.24) and highest for short-acting (RR=0.56, 95%CI 0.55-0.57). While prescribing rates for methadone decreased markedly from 2012-2013 to 2017-2018 in all demographic categories, the patient characteristics associated with methadone prescribing were similar between the two periods. In 2012-2013 and 2017-2018, females were less likely to be prescribed methadone than males (RR=0.66; 95%CI:0.55-0.81 and RR=0.58; 95%CI:0.45-0.76, respectively). Patients aged 50-64 years of age had the highest rate of methadone prescriptions compared to those in all other age categories; patients aged ≥65 had the highest prescription rates for other long-acting opioids. The methadone prescription rate was higher among non-Hispanic whites compared with all other racial/ethnic groups and this difference was more pronounced in the later time period. Conclusions: Methadone prescribing rates decreased across time, more so than for short-acting and other long-acting opioids. Demographics of patients prescribed methadone were similar across time.
Jack Westfall
jwestfall@aafp.org 11/19/2021very important topic. Great poster and abstract. Thanks for doing this research. and providing this care to patients.