PCR060: Rapid adaptation of cancer screening practices during COVID-19: A multi-state qualitative study
Karim Hanna, MD; Brandylyn Arredondo; Melody Chavez; Laura Szalacha; Shannon Christy, PhD, BA, MA; Susan Vadaparampil, PhD, MPH; Usha Menon, PhD; Jessica Islam, PhD, MPH; Young-Rock Hong, PhD, MPH; Amir Alishahi Tabriz, MD, PhD, MPH; Jennifer Kue, PhD; Kea Turner, PhD, MA, MPH
Abstract
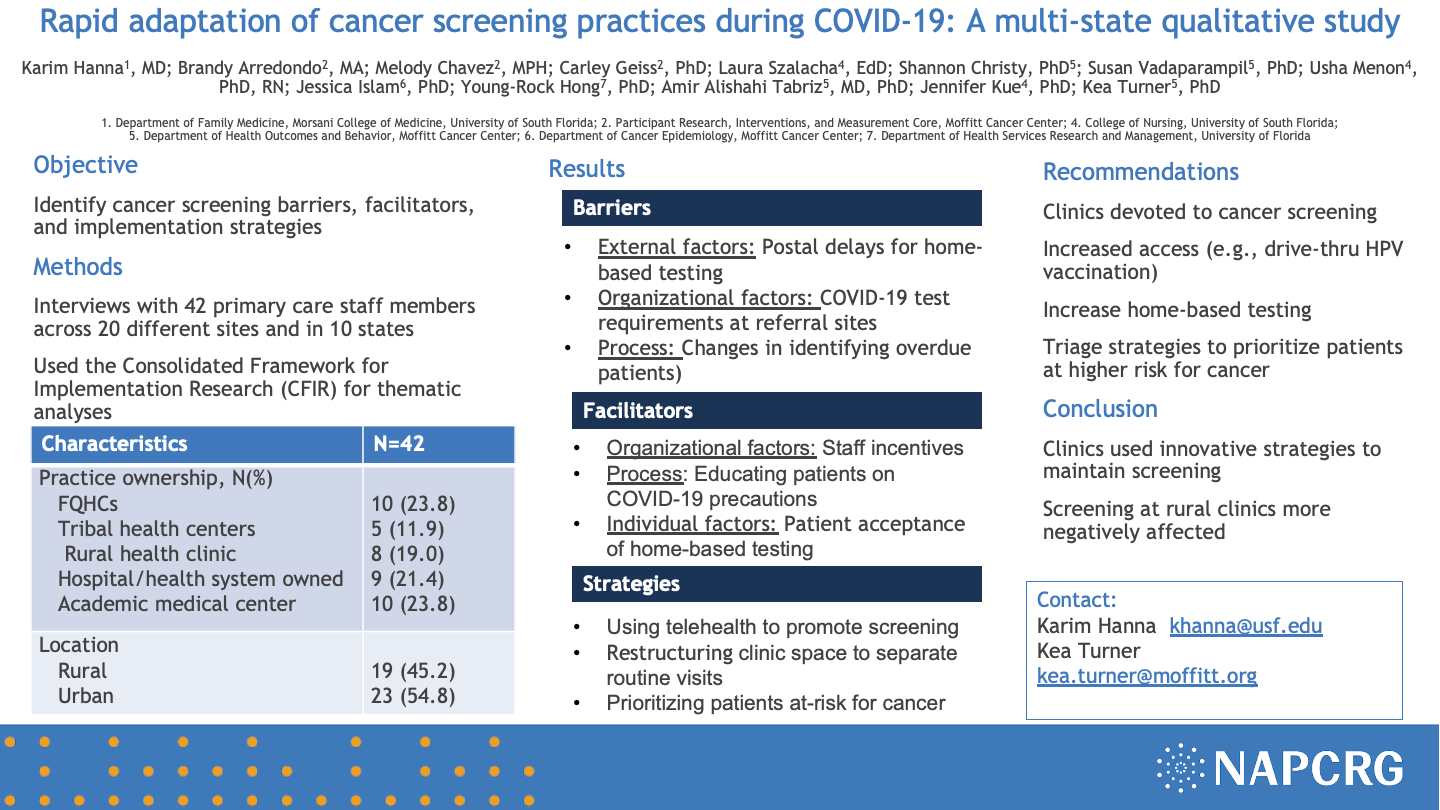
Objective: This study sought to: 1) identify cancer screening barriers and facilitators during the COVID-19 pandemic; 2) describe cancer screening adaptations; and 3) provide recommendations.
Study design: A qualitative study was conducted (n= 42) with primary care staff. Individual interviews were conducted through videoconference from August 2020 – April 2021 and recorded, transcribed, and analyzed for themes using NVivo 12 Plus.
Setting: Primary care practices included federally qualified health centers, tribal health centers, rural health clinics, hospital/health system-owned, and academic medical centers located across ten states including urban (55%) and rural (45%) sites.
Population studied: Primary care staff included physicians (n=13), residents (n=10), advanced practice providers (n=9), and administrators (n=10).
Outcome measures: The interviews assessed perceptions about cancer screening barriers and facilitators, necessary adaptations, and future recommendations.
Results: Barriers to cancer screening included delays in primary and specialty care, staff shortages, lack of personal protective equipment, patient hesitancy to receive in-person care, postal service delays for mail-home testing, COVID-19 travel restrictions (for Mexico-US border-crossing patients) and organizational policies (e.g., required COVID-19 testing prior to screening). Facilitators included better care coordination and collaboration due to the pandemic and more time during telehealth visits to discuss cancer screening compared to in-person visits. Adaptations included delayed screening, patient triage (e.g., prioritizing patients overdue for screening), telehealth visits to discuss cancer screening, mail-home testing, coordinating cancer screenings (e.g., providing fecal immunochemical test materials during cervical cancer screening) and same-day cancer screening. Recommendations included more public health education about the importance of cancer screening during COVID-19, more mail-home testing, and expanded healthcare access (e.g., weekend clinic) to address patient backlogs for cancer screening.
Conclusions: Primary care staff developed innovative strategies to adapt cancer screening during the COVID-19 pandemic. Unresolved challenges (e.g., patient backlogs) will require additional implementation stra
Jack Westfall
jwestfall@aafp.org 11/20/2021This is a great topic and research study. Nice work. Thanks