SRFP053: Hotspotting in Primary Care: An Interdisciplinary Model for Medically Complex, Socially At-Risk Patients (Pearls)
Veronica Daniel; Glenda Sundberg, FNP
Abstract
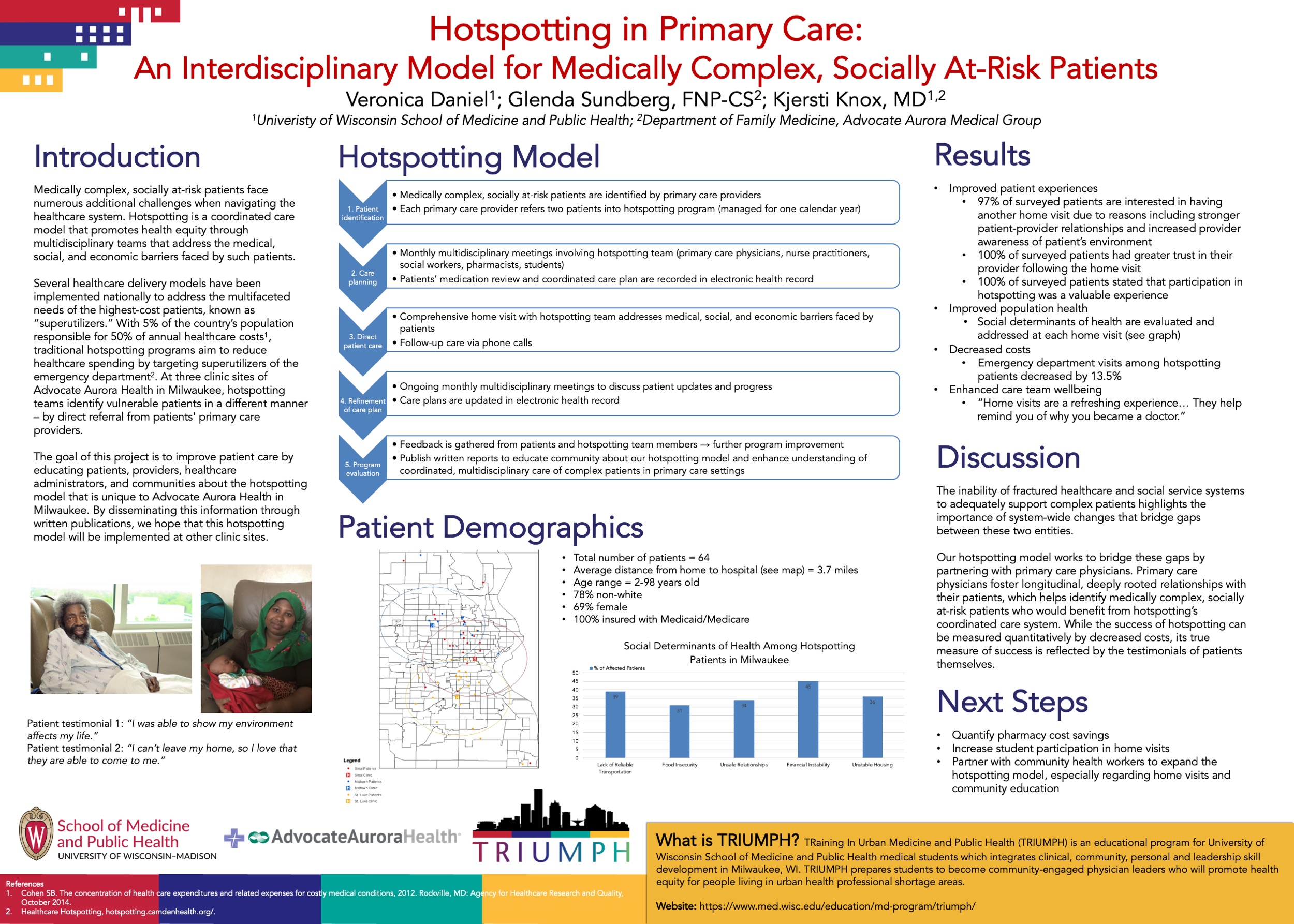
Context: Medically complex, socially at-risk patients face numerous additional challenges when navigating the healthcare system. Hotspotting is a coordinated care model that promotes health equity through multidisciplinary teams that address the medical, social, and economic barriers faced by such patients. Several healthcare delivery models have been implemented nationally to address the multifaceted needs of the highest-cost patients, known as “superutilizers.” Traditional hotspotting programs aim to reduce healthcare spending by targeting superutilizers of the emergency department. At three clinic sites of Advocate Aurora Health in Milwaukee, hotspotting teams identify vulnerable patients in a different manner – by direct referral from patients' primary care providers.
Objective: The goal of this project is to improve patient care by educating patients, providers, healthcare administrators, and communities about the hotspotting model that is unique to Advocate Aurora Health in Milwaukee. By disseminating this information through written publications, we hope that this hotspotting model will be implemented at other clinic sites.
Study Design: Qualitative study.
Setting/Dataset/Population Studied: The study setting includes patients from three family medicine clinics in the Advocate Aurora Health system in Milwaukee. Primary care providers from these clinics identify patients with multiple chronic comorbidities and/or socioeconomic challenges and refer them into the hotspotting program. 64 patients were included in this study, all of whom are residents of Milwaukee and are insured with either Medicaid or Medicare.
Results: 1. Improved patient experiences (97% of patients are interested in having another home visit, 100% had greater trust in providers). 2. Improved population health (social determinants of health are evaluated and addressed at each home visit). 3. Decreased costs (ED visits among hotspotting patients decreased by 13.5%). 4. Enhanced care team wellbeing.
Conclusions: The inability of fractured healthcare and social service systems to adequately support complex patients highlights the importance of system-wide changes that bridge gaps between these two entities. Our hotspotting model works to bridge these gaps by partnering with primary care physicians. While the success of hotspotting can be measured quantitatively by decreased costs, its true measure of success is reflected by the testimonials of patients themselves.
Objective: The goal of this project is to improve patient care by educating patients, providers, healthcare administrators, and communities about the hotspotting model that is unique to Advocate Aurora Health in Milwaukee. By disseminating this information through written publications, we hope that this hotspotting model will be implemented at other clinic sites.
Study Design: Qualitative study.
Setting/Dataset/Population Studied: The study setting includes patients from three family medicine clinics in the Advocate Aurora Health system in Milwaukee. Primary care providers from these clinics identify patients with multiple chronic comorbidities and/or socioeconomic challenges and refer them into the hotspotting program. 64 patients were included in this study, all of whom are residents of Milwaukee and are insured with either Medicaid or Medicare.
Results: 1. Improved patient experiences (97% of patients are interested in having another home visit, 100% had greater trust in providers). 2. Improved population health (social determinants of health are evaluated and addressed at each home visit). 3. Decreased costs (ED visits among hotspotting patients decreased by 13.5%). 4. Enhanced care team wellbeing.
Conclusions: The inability of fractured healthcare and social service systems to adequately support complex patients highlights the importance of system-wide changes that bridge gaps between these two entities. Our hotspotting model works to bridge these gaps by partnering with primary care physicians. While the success of hotspotting can be measured quantitatively by decreased costs, its true measure of success is reflected by the testimonials of patients themselves.