SRFP014: Behavioral health treatment barriers and preferences of primary care patients with chronic pain and alcohol use
Katherine Buckheit, PhD; Jacob Scharer, PhD; Travis Loughran, PhD; Gregory Beehler; Dezarie Moskal, PhD; Jennifer Funderburk, PhD
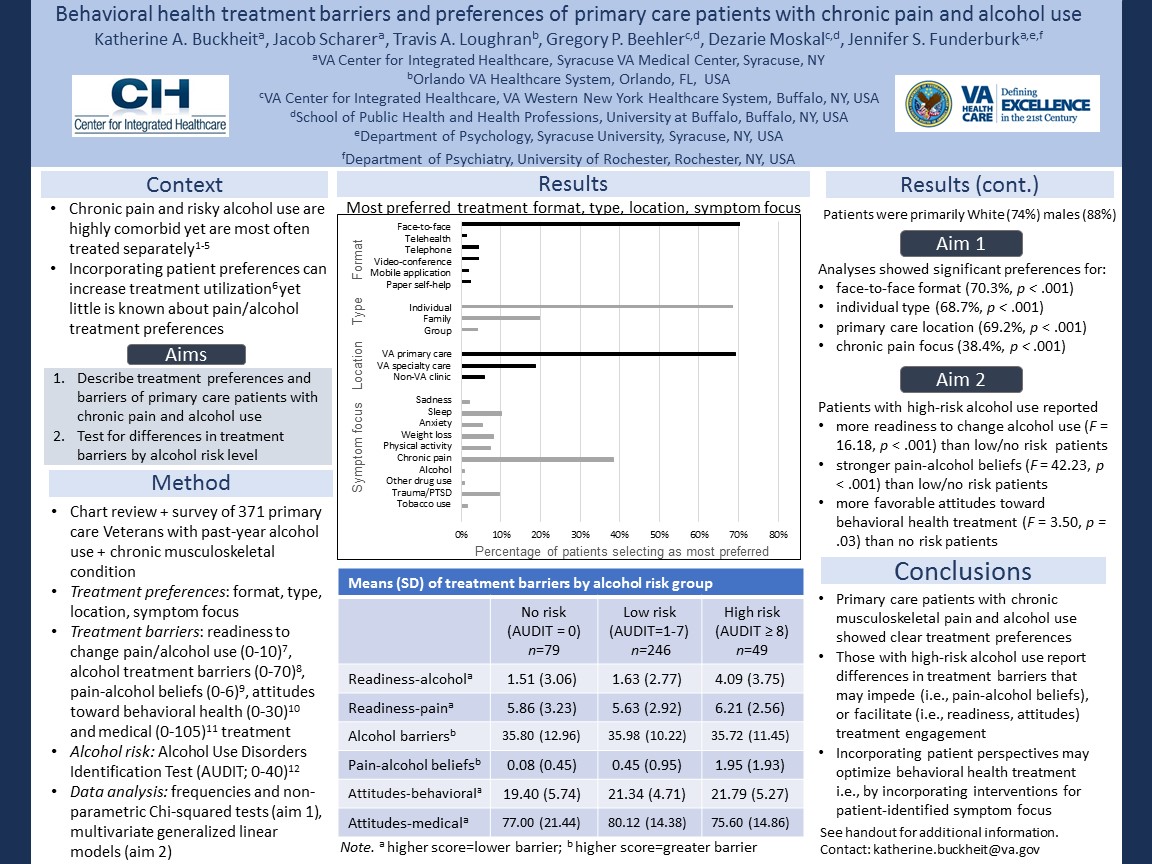
Context: Although chronic pain and high-risk alcohol use are prevalent in primary care and associated with more severe pain and functional impairment, current approaches address them separately and often neglect risky alcohol use among those with chronic pain. Treatments tailored to patient preferences increase utilization, yet little is known about patient treatment preferences for chronic pain and high-risk alcohol use. Objective: Describe treatment barriers and preferences of primary care patients with chronic musculoskeletal pain and past-year alcohol use and test for differences based on alcohol use (no risk, low risk, high risk). Study Design: Chart review and patient survey. Setting: VA primary care clinics. Inclusion criteria: ≥ 18 years old, past year VA primary care visit, chronic musculoskeletal condition, past year alcohol use. Exclusion criteria: psychotic or neurocognitive disorder diagnosis. Eligible participants were identified via chart review and mailed a survey packet. Population Studied: Participants (N = 371) were primarily White (74.7%) male (88.4%) veterans. Main and Secondary Outcome Measures: Readiness to change, alcohol treatment barriers, pain-alcohol beliefs, attitudes toward behavioral health and medical treatment, and treatment preferences were assessed. Results: Chi-square tests revealed statistically significant preferences for: face-to-face (70.3% preferred), individual (68.7% preferred), VA primary care, (69.2% preferred), and chronic pain focus (38.4% preferred). Patients with high-risk alcohol use reported more readiness to change alcohol use, stronger pain-alcohol beliefs, and more favorable attitudes toward behavioral health treatment than those with low- or no-risk alcohol use. Conclusion: Primary care patients with chronic musculoskeletal pain and alcohol use showed clear preferences for individual, face-to-face behavioral health treatment focused on chronic pain in a VA primary care clinic. Those with co-occurring high-risk alcohol use may experience differences in treatment barriers that may impede treatment engagement (i.e., stronger pain-alcohol beliefs), and in other cases, may facilitate treatment engagement (i.e., more readiness to change, more favorable treatment attitudes) compared to those with low- or no-risk alcohol use. Incorporating patient perspectives may help clinicians provide optimal behavioral health treatment for chronic pain and/or hazardous alcohol use in primary care.
Jack Westfall
jwestfall@aafp.org 11/21/2021Great poster and abstract. thanks