SRFP010: Assessment and management of allergy history with a novel mRNA vaccine
Christina Holt, MD, MSc; Jesse Butler; Katie Sharp, MD; John McDonald
Abstract
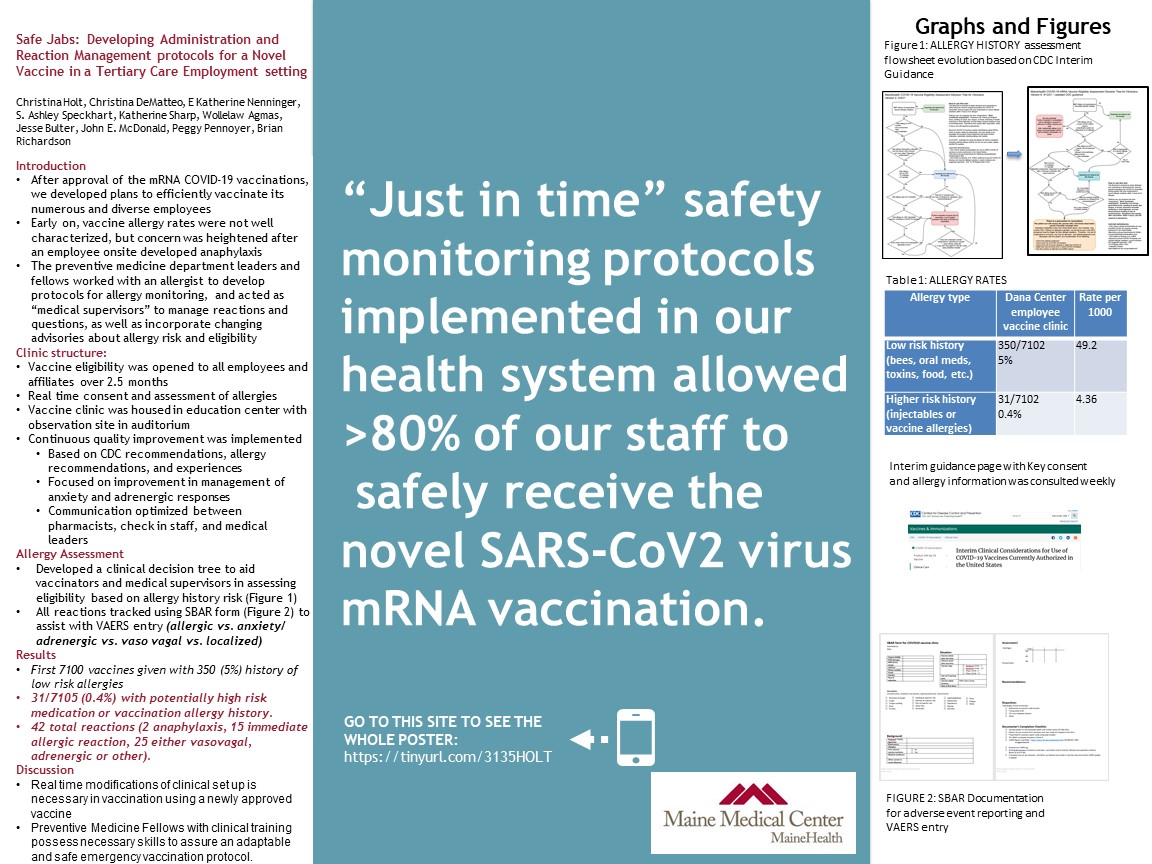
Context: Tertiary care hospital provided onsite COVID-19 vaccine roll out as a work benefit for all care team members with medically supervised waiting period at the time of the distribution of the first round of the novel mRNA COVID-19 vaccines. Little was known about the immediate hypersensivity reactions or what might predispose to cross reactivity.
Objective: We developed a working protocol to continuously track the vaccines administered, the patient history of allergy and hypersensistivity, the reactions observed and the care plan developed (determination of allergy to mRNA vaccines or normal vaccine response). Continuous process improvement allowed us to change protocols as the CDC developed guidance. Every patient was observed for at least 15 minutes and every reaction was reviewed by a physician supervising the waiting area. We aimed to determine if there were predictors of adverse, immediate reaction to the vaccine and to assess prevalence of risk factors (history of allergy to polyethylene Glycol or polysorbate; allergy to other injectable medication or vaccines; hypersensitivity to multiple substances).
Study Design: cohort study of all employees who received a first mRNA COVID-19 vaccine between December 16 and January 7th. Descriptive statistics were developed with demographic and medical history recorded, reactions noted and treatment given.
Setting or Dataset: tertiary care hospital in urban area
Population Studied: employees who received an mRNA COVID-19 vaccine
Intervention/Instrument: clinical records from employee vaccine clinic;
Outcome Measures: record of immediate response, determination of allergy;
Results: we served over 7000 individuals with approximately 10% having a history of anaphylactic reaction. We had fewer with history of anaphylaxis to medications or vaccines. We delivered these vaccines safely, and observed three cases of immediate anaphylaxis on first dose of mRNA and over 50 cases of immediate allergic hypersensitivity. We did not see any patterns that predicted these reactions (gender, age or medical history).
Expected Outcomes: We used this data to inform our employee health vaccination campaign and to inform the health system as strategies and safety protocols for vaccination of the population were developed.
Objective: We developed a working protocol to continuously track the vaccines administered, the patient history of allergy and hypersensistivity, the reactions observed and the care plan developed (determination of allergy to mRNA vaccines or normal vaccine response). Continuous process improvement allowed us to change protocols as the CDC developed guidance. Every patient was observed for at least 15 minutes and every reaction was reviewed by a physician supervising the waiting area. We aimed to determine if there were predictors of adverse, immediate reaction to the vaccine and to assess prevalence of risk factors (history of allergy to polyethylene Glycol or polysorbate; allergy to other injectable medication or vaccines; hypersensitivity to multiple substances).
Study Design: cohort study of all employees who received a first mRNA COVID-19 vaccine between December 16 and January 7th. Descriptive statistics were developed with demographic and medical history recorded, reactions noted and treatment given.
Setting or Dataset: tertiary care hospital in urban area
Population Studied: employees who received an mRNA COVID-19 vaccine
Intervention/Instrument: clinical records from employee vaccine clinic;
Outcome Measures: record of immediate response, determination of allergy;
Results: we served over 7000 individuals with approximately 10% having a history of anaphylactic reaction. We had fewer with history of anaphylaxis to medications or vaccines. We delivered these vaccines safely, and observed three cases of immediate anaphylaxis on first dose of mRNA and over 50 cases of immediate allergic hypersensitivity. We did not see any patterns that predicted these reactions (gender, age or medical history).
Expected Outcomes: We used this data to inform our employee health vaccination campaign and to inform the health system as strategies and safety protocols for vaccination of the population were developed.