PRP019: COVID Challenge: Are we just phoning in?
Yun Shi, MD, PhD; Fehima Dawy; Inez Cruz, PhD, MSW; Hyunyoung Kim, MD, MPH; Esther Shin; Jordan Kampschmidt; Marcy Wiemers, MD; Samantha Baginski; Lauren Fuller, MD
Abstract
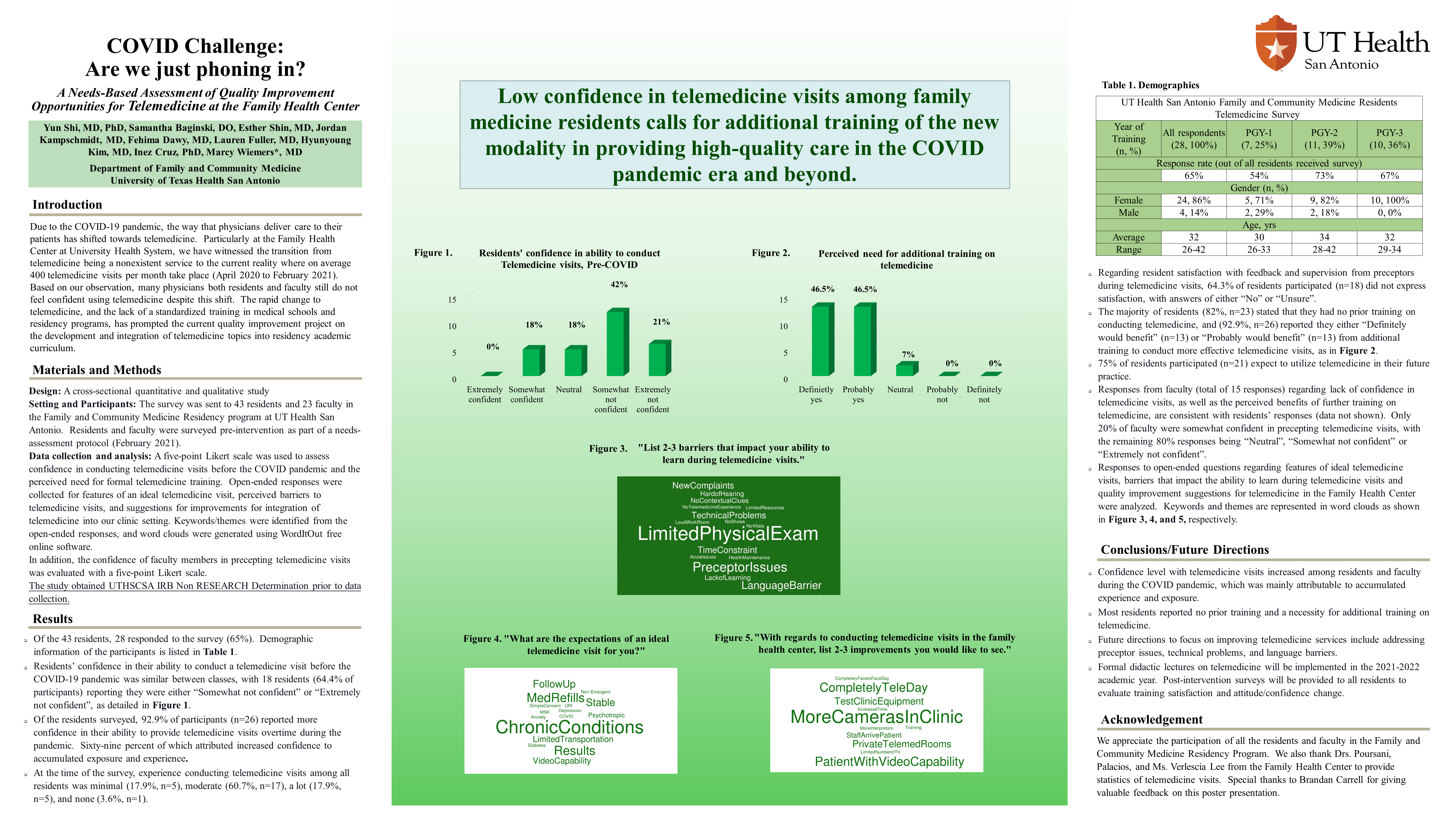
Context: The COVID-19 pandemic has expedited the shift towards telemedicine as a way physicians deliver care to their patients. However, many physicians do not feel confident practicing telemedicine due to the rapid change and lack of standardized training. Objective: To develop and integrate telemedicine curriculum into the UT Health San Antonio Family Medicine Residency program. Study Design: A cross-sectional quantitative and qualitative study. Setting and Participants: A pre-intervention survey as part of a needs assessment was sent to 43 residents in the UT Health San Antonio Family Medicine Residency program. Data and Analysis: A five-point Likert scale was used to assess the confidence level in conducting telemedicine visits and the perceived need for formal telemedicine training. Open-ended responses were collected to identify features of an ideal telemedicine visit, barriers to telemedicine visits, and areas of improvement in conducting telemedicine within the program. Word clouds were generated from the keywords and themes identified from the responses. Results: Among the 28 residents who completed the survey, 64% (n=18) reported they were not confident at the beginning of the COVID-19 pandemic. However, 93% (n=26) reported their confidence increased over time, mostly from accumulated exposure and experience. The majority of residents stated they had no prior training in telemedicine (82%; n=23) and would benefit from additional training (93%; n=26). 75% of the residents (n=21) expected to utilize telemedicine in their future practice. Common themes identified from the responses to the open-ended questions include follow-ups for low-moderate medical complexity, barriers in physical exams, supervision, language, and improvement in technology. Conclusions and Future Directions: Most residents reported the need for additional training on telemedicine. Future ways of improving telemedicine services include addressing precepting issues, technical problems, and language barriers. Formal didactic lectures on telemedicine will be implemented in the 2021-2022 academic year, and a post-intervention survey will be conducted to assess training satisfaction, confidence improvement.
Jack Westfall
jwestfall@aafp.org 11/21/2021Terrific project. Great poster and abstract. Thanks for sharing at NAPCRG