PRP057: Mindful Eating Healthy Nutrition Group Visit Intervention for Adult Metabolic Syndrome Feasibility Acceptability for Patients
Leonard Finn, MD; Jennifer Carroll, MD, MPH; Elisabeth Callen, PhD; Lauren Kiel; Erin Callister; Ashley Kiel; Meredith Shefferman, PhD; Carrie Landin, PsyD; Lauren Grossman
Abstract
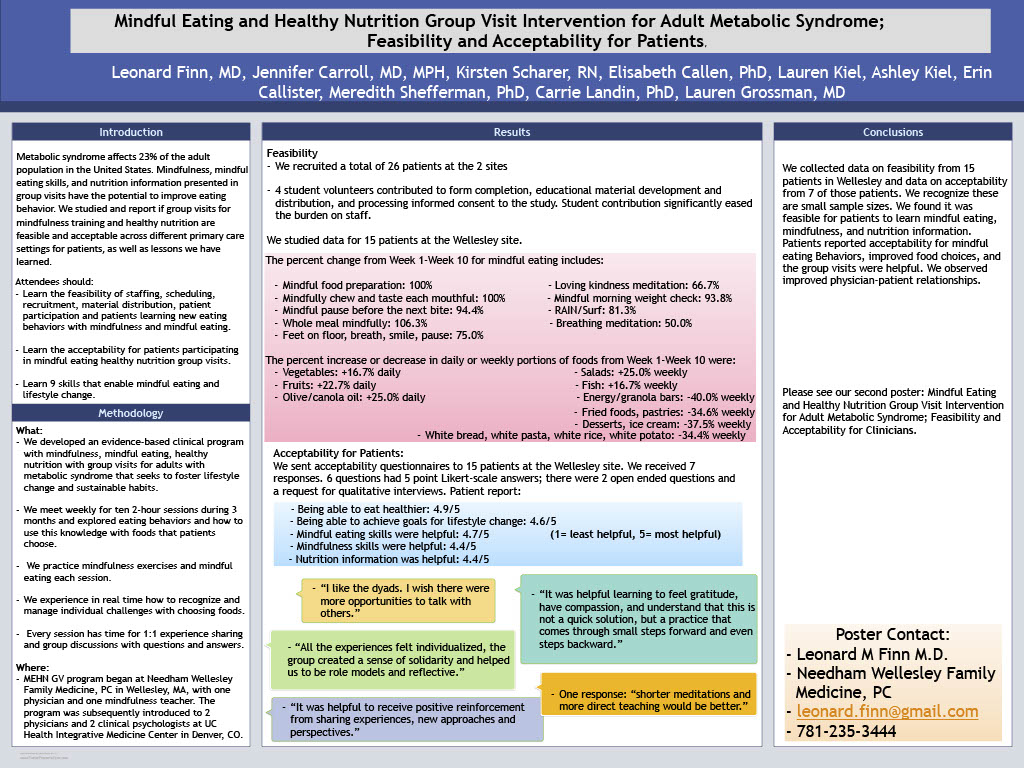
Context: Metabolic syndrome, a cluster of risk factors including elevated fasting glucose, high triglycerides, and hypertension, low HDL and abdominal obesity, affects 23% of adult population in the United States. People with metabolic syndrome are at high risk for diabetes and cardiovascular disease and have higher all-cause mortality. Usual treatment for metabolic syndrome is weight loss through diet and exercise. Evidence supports the use of mindfulness as a strategy for effective weight management. Objective: Are group visits for mindful eating and healthy nutrition education feasible and acceptable across different primary care settings for patients, staff and clinicians? Study design: Pilot/feasibility study. Setting: 1group - Needham Wellesley Family Medicine PC, a physician-owned family medicine practice in Wellesley, MA. Population Studied: 15 patients 18+ years with obesity/overweight and metabolic syndrome or diabetes, cardiovascular disease, hypertension. actively enrolled at site, able to consent, understand procedures, Exclusions: lack cognitive capacity, unable/unwilling to consent or complete study. Intervention: Group visits with mindfulness, mindful eating, healthy nutrition for adults with metabolic syndrome and related conditions. Curriculum: evidence-based principles of mindfulness, mindful eating, healthy nutrition, and activity to improve patient management of metabolic syndrome and related conditions. The curriculum seeks to foster sustainable lifestyle change related to eating behaviors, nutrition choices, activity, self-efficacy, stress-management, and goal setting. Physician, mindfulness teacher and patients meet for group visits weekly for ten weeks and 3 monthly visits. Outcome measures: patient surveys at T0, weeks 5 and 10. measure weight, blood pressure, mindfulness, mindful eating, nutrition practices. survey questions and semi-structured interviews after the sessions ended. We collected feasibility data for scheduling, staffing, recruiting patients, and for patients acquiring skills and knowledge; and acceptability to patients; Results: Patients report: being able: to eat healthier 4.5/5, and to achieve goals for lifestyle change 4.2/5; mindful eating was helpful 4.7/5; they have reinforcement from shared experiences, request more direct teaching, have more opportunity to talk with others. Outcomes to be reported: additional feasibility & acceptability results.
Diane Harper
harperdi@med.umich.edu 11/21/2021outstanding work. This is an important topic that is not often highlighted! Thank you for sharing with us at NAPCRG.