PRP059: Pain Interference and Depression in Patients with Non-cancer Pain
Lauren Wilson, LCSW; Lisa Miller-Matero, PhD; Jeffrey Scherrer, PhD; Matthew Amick, MS; Joanne Salas, MPH; Kirsti Autio, LMSW; Patrick Lustman, PhD
Abstract
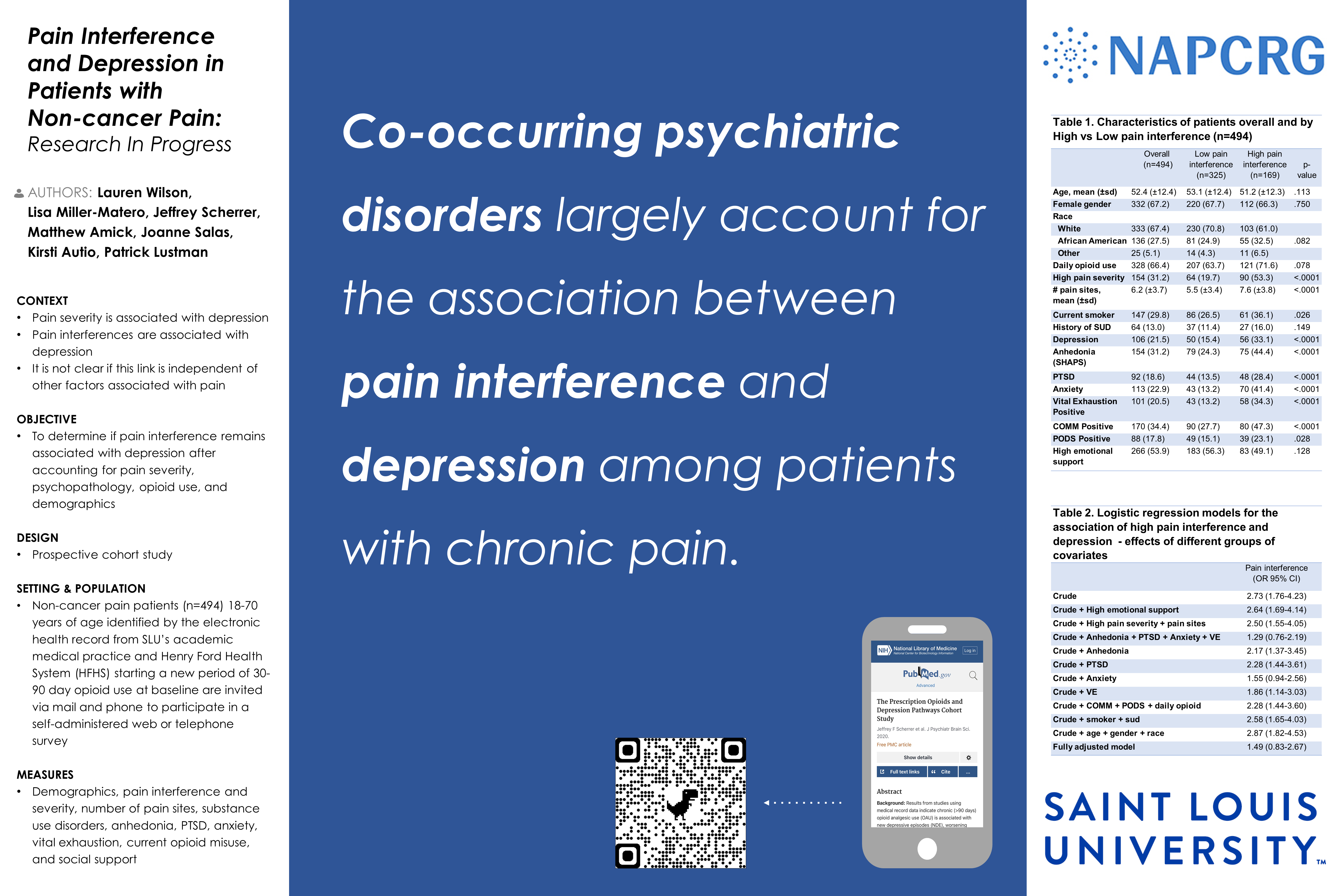
Context: As pain severity increases, symptoms of depression increase. However, pain related interference with functioning may have a stronger association with depression than pain severity. To improve pain management, it is important to elucidate the relationship between pain variables and depression. Objective: To determine if pain interference is associated with depression after controlling for pain severity, psychopathology, opioid use and demographics. Study Design: Prospective cohort study. Setting: Patients from Saint Louis University’s (SLU) academic medical practice and Henry Ford Health System (HFHS) identified by the electronic health record were invited via mail and phone to participate in self-administered web or telephone surveys. The present study used data from the first 494 patients who completed the baseline assessment and had complete data on all measures. Population: Non-cancer pain patients (n=494) 18-70 years of age starting a new period of 30 to 90 day opioid use (e.g. no use in past 3 months) at baseline. Outcome: DSM-5 criteria past-year depression diagnosis. Measures: Demographics, pain interference and severity, number of pain sites, substance use disorders, anhedonia, PTSD, anxiety, vital exhaustion, current opioid misuse, and social support. Results: In crude analysis, high vs. low pain interference was significantly associated with anhedonia, PTSD, generalized anxiety disorder, vital exhaustion and high risk for opioid misuse. Pain interference was associated with depression (OR=2.73; 95%CI:1.76-4.23) in crude models. This association remained after adjusting for high pain severity and number of pain sites. However, pain interference was no longer significantly associated with depression after adjusting for all covariates (OR=1.49; 95%CI:0.83-2.67). The effect of individual covariates on this association revealed that generalized anxiety disorder largely explained the association between pain interference and depression. Conclusions: Co-occurring psychiatric disorders largely account for the association between pain interference and depression. Longitudinal data collection will reveal whether comorbid psychopathology increases risk for high pain interference or whether high pain interference contributes to risk for psychopathology and comorbid depression. Screening for psychiatric disorders, not just depression, in patients with high pain interference may be warranted to identify undiagnosed conditions and emotional distress.
Diane Harper
harperdi@med.umich.edu 11/21/2021Thank you for sharing with us at NAPCRG.