PCR051: Perspectives from Primary Care Providers and Patients on the Role of Primary Care in the NASH Patient Journey
Elizabeth Tanner, PhD; Karl Nadolsky, DO; Donna Cryer, JD; Amy Articolo; Travis Fisher, PharmD; Jennifer Schneider, PharmD; Mary Rinella, MD
Abstract
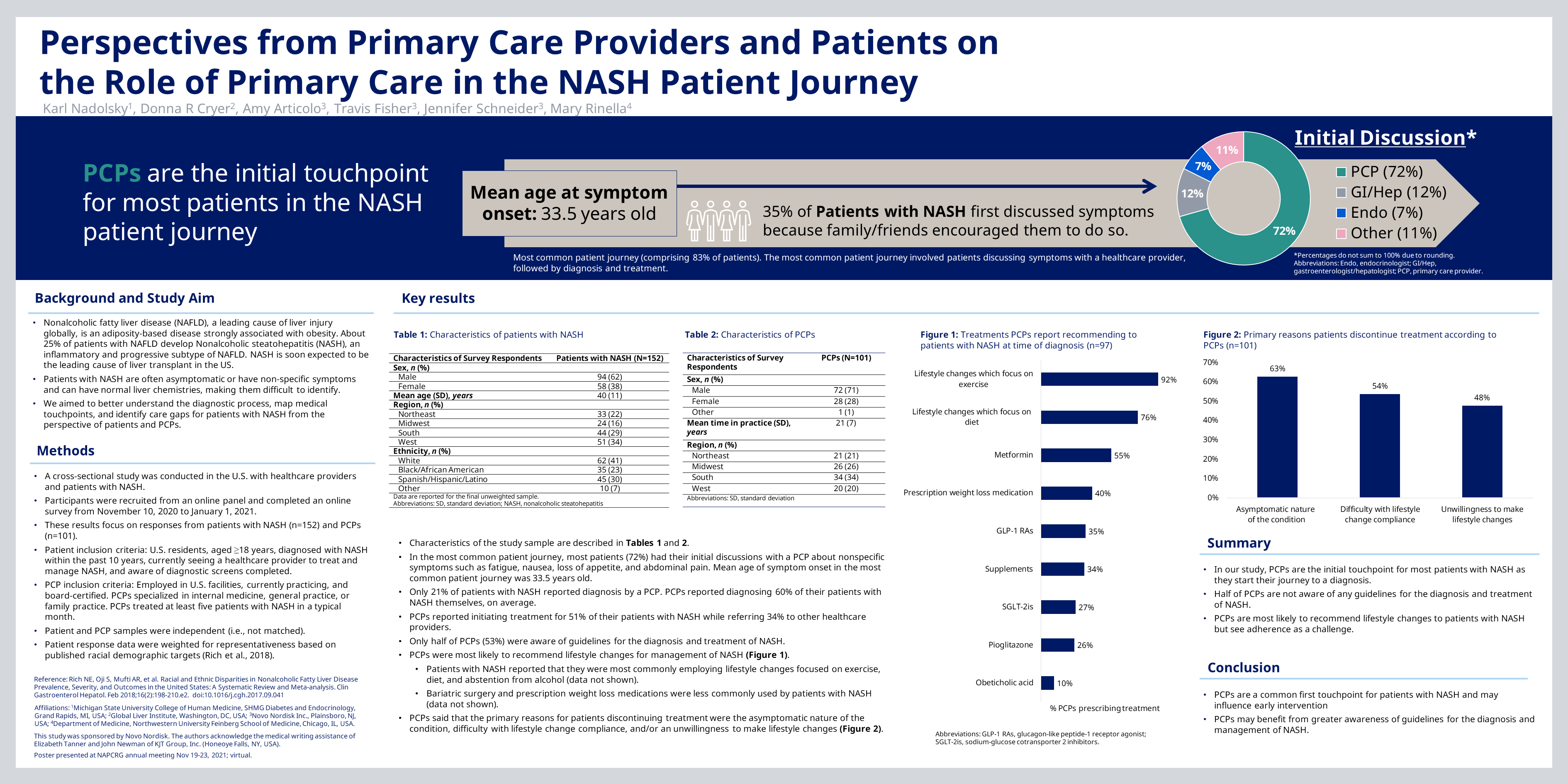
Context: Nonalcoholic fatty liver disease (NAFLD), a leading cause of liver injury globally, is associated with obesity and diabetes. About 25% of patients with NAFLD develop Nonalcoholic steatohepatitis (NASH), an inflammatory and progressive subtype of NAFLD that predisposes patients to cirrhosis, liver cancer, and is the most rapidly increasing indication for liver transplant. Patients with NASH (PwN) are asymptomatic or have non-specific symptoms and can have normal liver chemistries, making them difficult to identify. Primary Care Physicians (PCPs) can play an important role in identifying those at risk for NASH. Objective: To map the medical touchpoints and care gaps for PwN from the perspective of PwN and PCPs. Study Design: Cross-sectional study. Setting: Online survey in the U.S. Population studied: Patients aged 18-55 with self-reported NASH diagnosis currently seeing a healthcare provider (HCP) for NASH management. PCPs seeing >5 PwN monthly who report they are highly familiar with NASH. Outcome measures: Self-reported attitudes, experiences, and behaviors related to diagnosis and management of NASH. Results: Respondents included 152 PwN and 101 PCPs. Most (72%) PwN reported initial discussions occurred with PCPs. However, only 30% of PwN reported diagnosis by a PCP; this contrasts with PCP reports of diagnosing 60% of their patients themselves. PCPs reported initiating NASH treatment for 50% of patients and referring 32% to other HCPs. Treatments initiated at diagnosis by PCPs included lifestyle changes focused on exercise (92%) and diet (76%); other interventions were recommended less frequently: anti-obesity medications (40%), GLP-1 agonists (35%), pioglitazone (26%), or SGLT-2 inhibitors (27%). PwN reported treatment currently in use or previously used included exercise (94%), limiting alcohol/improving diet (88%); they were less frequently prescribed weight loss medication (57%) or bariatric surgery (31%). PCPs identified primary reasons their patients discontinued treatment as lack of symptoms (63%), difficulty with lifestyle change (54%), or unwillingness to make lifestyle changes (48%). Conclusions: PCPs are an important first touchpoint for PwN and can influence early intervention in NASH diagnosis and progression. Proactive discussion about the risks of NASH regardless of symptom presence should be considered. Improved guidelines on identifying and diagnosing patients to guide interactions in the primary care setting are needed.
Jack Westfall
jwestfall@aafp.org 11/20/2021Terrific poster and presentation. Thanks for your work.